A pulmonologist describes how using an esophageal balloon can provide a more precise diagnosis and hemodynamic classification of pulmonary hypertension
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Right heart catheterization is needed for the diagnosis and hemodynamic classification of pulmonary hypertension (PH). Pulmonary hypertension is defined as a mean pulmonary artery pressure of more than 20 mmHg. There are three major hemodynamic types of PH, including precapillary, postcapillary and combined pre and postcapillary PH. The diagnosis of both postcapillary and combined pre and postcapillary PH requires an elevated pulmonary artery wedge pressure (PAWP), which is defined as a value of 15 mmHg or above. Postcapillary and combined pre and postcapillary PH are commonly seen in conditions that affect the left heart, such as heart failure with preserved or reduced ejection fraction.1
The most common cause of PH is left heart disease, which is characterized by an elevated mean pulmonary artery and wedge pressures. Nevertheless, both pressures could appear elevated in patients with high intrathoracic pressure, such as those with obesity.2
We recently tested whether adjusting pulmonary pressures by intrathoracic pressure, using an esophageal balloon, allows for more precise diagnosis and hemodynamic classification of PH. In a cohort of obese patients with PH, we demonstrated that the true intravascular pressure (determination adjusted for intrathoracic pressure) reduced the diagnosis of PH by a quarter, and markedly decreased the diagnosis of postcapillary or combined pre- and postcapillary PH in patients with obesity.3
In our cohort of patients with obesity (body mass index = 44 ± 10 kg/m2), the esophageal pressure at end-expiration was 14 ± 4 mmHg (range: 6-25 mmHg). Therefore, when we adjusted for this determination, both the end-expiration mean pulmonary artery and wedge pressure were significantly reduced. This significant pressure correction leads to important implications as it may a) normalize pulmonary pressures and reduce anxiety, tests and treatments based on a PH disorder that patients may not have, and b) remove the diagnosis of postcapillary PH and prevent unnecessary diuretics or other treatments in favor of PAH-specific interventions in combined pre and postcapillary PH.
Advertisement
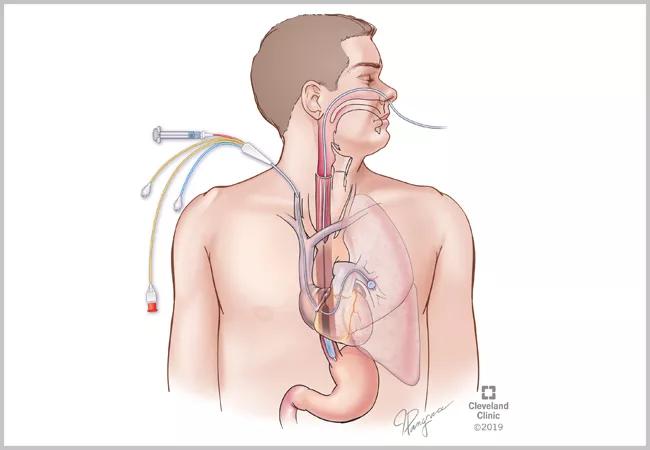
The measurement of the esophageal pressure is obtained by placing a flexible tube through the nose into the lower esophagus using local anesthetics (figure 1). Adequate position of the catheter is established by following certain criteria.3 The end-expiration esophageal pressure measurements can be obtained by the same hemodynamic system used to record the pulmonary pressures. Both end-expiration mean pulmonary and PAWP are then adjusted by the same absolute value (figure 2). Since pulmonary pressures are equally affected by the intrathoracic pressure, the adjustment by esophageal pressure does not affect the transpulmonary gradient (TPG: mean pulmonary artery – PAWP) or pulmonary vascular resistance (TPG/CO).
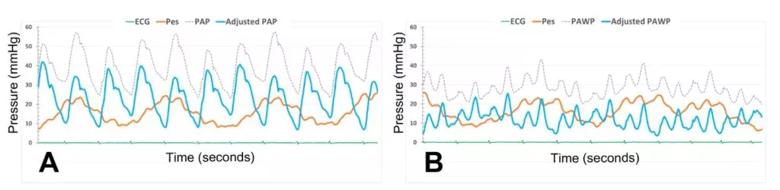
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8dfc1dcc-7b76-40ed-bec5-d4b62e6551ff/Tonelli-Figure-2-1024x250_jpg)
Figure 2: Impact of esophageal pressure determination on pulmonary vascular pressures.
Figure panels represent pressure recording of the pulmonary artery (panel A) and wedge (panel B) pressures. Panel A shows the pulmonary arterial pressure before (grey tracing) and after (blue tracing) adjustment for the esophageal pressure (Pes represented in red color). Panel B depicts the PAWP before (grey tracing) and after (blue tracing) adjustment for the esophageal pressure (Pes in represented in red color).
The measurement of esophageal pressure is important to determine the intrathoracic pressure in those patients for whom there is suspicion that this pressure might be elevated. The degree of obesity does not have a good correlation with the intrathoracic pressure. However, changing positions from supine to sitting reduces the intrathoracic pressure and its impact on the pulmonary pressure. It does not always reduce the end-expiration intrathoracic pressure to zero, however, and the vascular pressure reduction observed when sitting might be related to a lower preload due to pooling of blood in the lower extremities.
Advertisement
Clinical conditions with an increased intrathoracic pressure include obesity, chronic obstructive lung disease and asthma with air trapping, chest wall deformities and others. Hemodynamic indicators of increased intrathoracic pressure include an increased right atrial pressure, mean pulmonary artery pressure and PAWP with pronounced respiratory oscillations of pulmonary pressures.
We are currently testing other non-invasive tools that could predict with a good degree of accuracy the presence of higher intrathoracic pressure. A pretest probability of having a high intrathoracic pressure may help plan the esophageal balloon insertion in hemodynamic laboratories in which this intervention is not yet readily available. Alternatively, the determination of esophageal pressure, in supine position, and across the respiratory cycle, could also be done by gastroenterology as part of the esophageal manometry commonly performed in patients with achalasia.
In summary, adjusting pulmonary hemodynamics for esophageal pressure in patients with elevated intrathoracic pressure reduces the number of patients diagnosed with postcapillary PH. Measuring the esophageal pressure is relatively simple and should be considered in patients suspected of having high intrathoracic pressure, such as those with obesity, elevated mean pulmonary artery pressure and PAWP.
References
1. Sahay, S., G. Khirfan, and A.R. Tonelli, Management of combined pre- and post-capillary pulmonary hypertension in advanced heart failure with reduced ejection fraction. Respir Med, 2017. 131: p. 94-100.
Advertisement
2. Jawad, A., et al., Impact of Intrathoracic Pressure in the Assessment of Pulmonary Hypertension in Overweight Patients. Ann Am Thorac Soc, 2017. 14(12): p. 1861-1863.
3. Khirfan, G., et al., Impact of Esophageal Pressure Measurement on Pulmonary Hypertension Diagnosis in Obese Patients. Chest, 2022.
Advertisement
Advertisement

Recent breakthroughs have brought attention to a previously overlooked condition

A review of treatment options for patients who may not qualify for surgery

Looking at the real-world impact and the future pipeline of targeted therapies

The progressive training program aims to help clinicians improve patient care

New breakthroughs are shaping the future of COPD management and offering hope for challenging cases

Exploring the impact of chronic cough from daily life to innovative medical solutions

How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program

Collaborative patient care, advanced imaging techniques support safer immunotherapy management