Three-step treatment improves outcomes in difficult-to-treat liver cancer
Perihilar cholangiocarcinoma (PC) is a rare form of liver cancer that originates in the epithelial cells of the bile duct. It is associated with poor outcomes and a high morbidity rate because most patients present with advanced-stage disease at diagnosis. Treatment of PC is further complicated by involvement of both bile ducts, which makes the tumor unamenable to surgical resection. Outcomes of liver transplant alone are likewise poor unless the tumor is first treated properly. A multimodal approach of highly specialized radiation and chemotherapy followed by liver transplant has been shown to result in extremely promising outcomes in this difficult-to-manage disease.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Kevin Stephans, MD, Department of Radiation Oncology, shares his experiences with treating localized PC with a three-step approach that involves hyperfractionated radiotherapy, intrabiliary brachytherapy and liver transplant.
Dr. Stephans: Hyperfractionated radiotherapy refers to the delivery of very small radiation treatments (1.5 Gray per fraction) in two separate daily doses. This approach allows the normal tissue that surrounds PC to heal after an initial radiation dose. We then deliver a second dose of radiation before the tumor has the opportunity to fully recover.
For distinction, a standard radiation dose is approximately 2 Gray per fraction. For liver metastases, intrahepatic cholangiocarcinoma or hepatocellular carcinoma that arises in the liver we use hypofractionated radiation which delivers focused, large doses of radiation (about 7 to 15 Gray per fraction) to the tumor. But for pretransplant patients with cholangiocarcinoma that affects both bile ducts this is not an option, because high doses of radiation would likely cause damage or scarring of the bile ducts and other adjacent sensitive tissue. Hyperfractionated radiation allows an aggressive dose to be delivered to the tumor, while remaining gentle to the surrounding normal tissue.
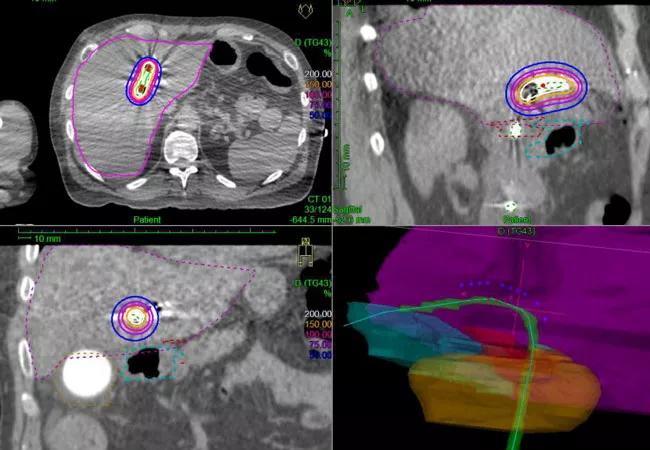
Dr. Stephans: We typically use intensity-modulated radiation therapy (IMRT) as the delivery method because it allows us to focus the radiation beam on the tumor and reduce the intensity of radiation to the surrounding healthy tissues. IMRT also delivers radiation at the most geometrically and anatomically favorable angles. The use of multiple beams creates a stronger focal point of radiation, sparing the surrounding normal tissues.
Advertisement
Dr. Stephans: In clinical trials conducted in patients with small cell lung cancer, twice-per-day hyperfractionated radiotherapy resulted in better short-term tumor control and less long-term side effects due to dose splitting. Side effects typically associated with standard radiotherapy of the liver include fatigue, nausea, vomiting and appetite suppression. However, in our clinical experience with hyperfractionated radiotherapy to date, we found it to be exceptionally tolerable. The patients typically report minimal side effects during the first few days of treatment, and often even continue to work throughout its duration, which is truly amazing.
Furthermore, when combined with intrabiliary brachytherapy, our patient outcomes have shown that radiation is able to completely ablate the cholangiocarcinoma about 70 to 80 percent of the time, leaving no residual tumor in most patients. However, a liver transplant is still required after radiotherapy, because radiation can cause stricture of the bile ducts over the long term.
Dr. Stephans: Perihilar cholangiocarcinoma treatment is a three-step process. External hyperfractionated radiotherapy is delivered twice per day, Monday through Friday, for three weeks. Approximately one week after completing external radiation, the patients are admitted for three days and given high-dose brachytherapy, which is delivered internally from within the bile ducts.
In this step, one access catheter is placed in the right bile duct and another in the left bile duct, and a source of radiation is placed inside both catheters. The source delivers radiation at 10 to 15 different positions inside the tumor, and the tumor ultimately receives a very large cumulative dose of radiation.
Advertisement
With the initial 30 external treatments, we are treating the edges of the tumor and the surrounding lymph nodes, while the final three high-precision, high-dose treatments are delivered to the tumor internally.
Throughout the three-week external radiation treatment, the patients are given radiation-sensitizing chemotherapy. Chemotherapy is not given during brachytherapy but is then reintroduced while the patient awaits liver transplant, which is the final treatment step.
Dr. Stephans: Given the rarity of PC, the standard of care is always evolving; however, this approach of hyperfractionated radiation, intrabiliary brachytherapy and liver transplant is associated with excellent survival, and is the preferred approach for patients with PC who are candidates for aggressive treatment.
Cholangiocarcinoma affecting both bile ducts is very rare, and treatment approaches are evolving, so it is difficult to answer this question. What we can say from our clinical experience at Cleveland Clinic is that hyperfractionated radiotherapy, combined with brachytherapy and liver transplant, results in improved survival and outcomes of patients with PC.
Dr. Stephans: This multidisciplinary approach requires coordination between five medical teams including hepatobiliary surgery, hepatology, medical oncology, radiation oncology and interventional radiology, and can best be delivered in the scope of a large medical center. Given the high degree of specialized coordination of care required, referring patients to a high-volume transplant center that has experience with all aspects of care for PC is the best option.
Advertisement
Advertisement

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Structured interventions enhance sleep, safety and caregiver resiliency in high-acuity units

Addressing rare disease and challenging treatment course in an active young patient