Modification of traditional staging factors associated with survival in high-risk disease
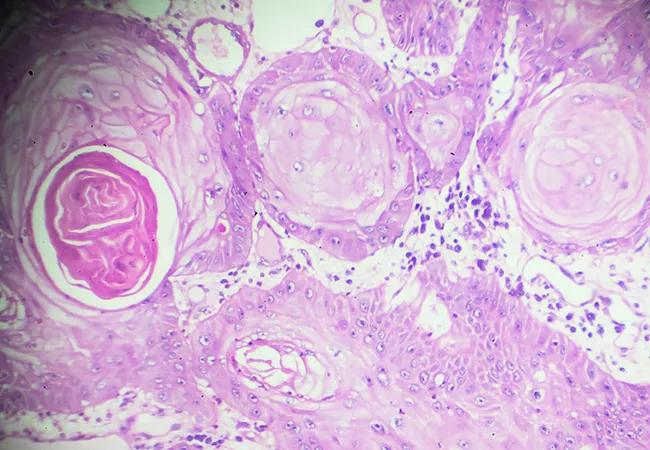
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/700de295-9539-4807-a73a-366932d1ead8/21-CNR-2495664-CQD-650x450-1_jpg)
Squamous Cell carcinoma under microscopy
The process of staging cutaneous squamous cell carcinoma (CSCC) is typically done using the American Joint Commission on Cancer (AJCC) and Brigham and Women’s Hospital (BWH) tumor classification systems and is based on tumor factors alone. Cleveland Clinic researchers are attempting to update and expand upon that protocol using recursive partitioning analysis (RPA), a non-parametric modeling technique. Results of a new study on RPA were presented at the annual conference of the American Society for Radiation Oncology in October 2021.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The RPA, which focused on predicting survival in patients with high-risk CSCC, identified four prognostic subgroups. Researchers found that in addition to age, lymphovascular space invasion (LVSI), perineural invasion (PNI), burden of nodal metastasis and immunosuppression status were associated with recurrence-free survival (RFS) and overall survival (OS).
“Although surgery is often curative for CSCC, the disease recurs in a small number of patients,” explains Shlomo Koyfman, MD, Director of the Head & Neck Cancer Program at Cleveland Clinic. “Our goal was to figure out which factors would help identify that ‘needle in a haystack’ — patients who might benefit from additional therapies. We believe our results have implications for patient counseling, clinical trial design and post-treatment surveillance.”
A total of 444 patients with 523 primary tumors with BWH stage T2B and T3 CSCC were enrolled in the study. All had received definitive therapy, 76% were male, and 95% were White. The cohort had a median age of 74 years, and 31% were immunosuppressed.
Among the primary tumors, 12% were node-positive, 32% were node-negative and 56% had unknown nodal status. CSCC recurred in one-third of study participants.
The researchers performed a Kaplan-Meier analysis and logrank test to estimate and compare RFS and OS in the study population. The RPA was then performed to identify prognostic factors for the two outcomes.
“Our goal was not to change the BWH system but rather explore stratification in a large, robust, modern cohort for which data on radiation were available. This allowed us to obtain a more precise assessment of risk,” says Dr. Koyfman.
Advertisement
The authors found that immunosuppression, tumor recurrence, PNI and LVSI were associated with significantly worse RFS OS was predicted to be significantly worse in patients with immunosuppression, lymph node positivity and extranodal extension (ENE).
Four prognostic subgroups had distinct RFS patterns (P<0.0001). Class I included 212 patients aged less than 77 years without LVSI (63% RFS, 95% CI 56%-70%). Class II included 132 patients aged 77 years or more with no PNI (44% RFS, 95% CI 3%-55%). Class III included 36 patients aged less than 77 years with LVSI (2-year RFS 29%, 95% CI 17%-50%). Class IV included 60 patients aged 77 years or more (2-year RFS 25%, 95% CI 15%-41%).
Four prognostic subgroups also showed distinct OS patterns (P<0.0001). Class I included 141 patients aged less than 78 years with one or more positive lymph nodes (2-year OS 84%, 95% CI 79%-90%). Class II included 141 patients aged 78 years or more with no immunosuppression from chronic lymphocytic leukemia (CLL) (2-year OS 64%, 95% CI 55%-73%). Class III included 48 patients aged less than 78 years with more than one positive lymph node (2-year OS 54%, 95% CI 41%-71%). Class IV included 34 patients aged 78 years or more with immunosuppression from CLL (2-year OS 37%, 95% CI 23%-57%).
“The biggest lesson we learned from this analysis is that survival may not be the best endpoint in this population because patients with CSCC tend to be elderly. The risk of recurrence is much more important,” explains Dr. Koyfman. “We had expected that PNI, LVSI and ENE would predict worse outcomes, but our finding on immunosuppression may be somewhat controversial.”
Advertisement
In an updated iteration of their work on the RPA, Cleveland Clinic researchers and their collaborators at Brigham and Women’s hospital combined their data to perform a new analysis of CSCC recurrence. Their preliminary unpublished results provide updated estimates of recurrence in a more modern cohort and demonstrate that adjuvant radiation therapy significantly reduces the risk of recurrence in patients with BWH stages T2b and T3 disease. The team is also enrolling patients with CSCC in a prospective trial assessing Castle Biosciences’ DecisionDx-SCC gene expression profile test as a biomarker for recurrence. (Dr. Koyfman is an unpaid advisor to the company.)
“Although the BWH system has been available for years, our intent is to complement it with newer data,” explains Dr. Koyfman. “Our hope is to determine more rationally which patients benefit from radiation and incorporate the biomarkers we’ve identified into treatment, counseling and the design of the next generation of clinical trials.”
Advertisement
Advertisement
Goal-of-care discussions drive earlier hospice access
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting