Transperineal ultrasound a viable, non-invasive option for monitoring intra-fractional prostate motion

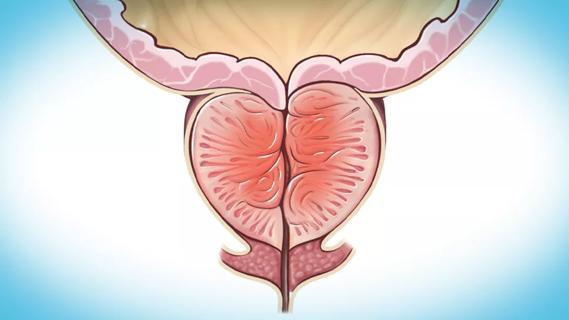
Research led by a team of Cleveland Clinic experts demonstrates the feasibility and clinical efficiency of ultrasound-guided prostate stereotactic body radiation therapy using a 4D transperineal ultrasound system.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These findings, which were recently published in the Journal of Applied Clinical Medical Physics, suggest that real-time intra-fraction motion management could help improve delivery accuracy for prostate stereotactic body radiotherapy.
“Ultra-hypofractionated stereotactic body radiotherapy for prostate cancer is an emerging treatment approach for low/intermediate-risk prostate cancer,” says first author Bingqi Guo, PhD, a medical physicist at the Department of Radiation Oncology at Taussig Cancer Institute, Cleveland Clinic. “Given the high precision nature of this treatment, it is important that the prostate stays in the same position.
“One way this is accomplished is with the use of fiducial markers; however, this is invasive and not a suitable option for all patients,” she continues. “In our study, we sought to better understand the potential of ultrasound-guided prostate SBRT, particularly for patients who would benefit from a more non-invasive approach.”
In this prospective study, Dr. Guo and her colleagues highlight their clinical experience using a transperineal ultrasound system as a means to monitor intra-fractional prostate motion for prostate stereotactic body radiotherapy (SBRT).
The analysis included 23 SBRT patients who were treated at the Cleveland Clinic between April 2016 and November 2019. Eligible patients were adults with an established diagnosis of prostate cancer who were proceeding with definitive radiation. They had a performance status of Karnofsky PS ≥ 70.
Advertisement
The research team used the following prescription doses: 36.25 Gy to the low-dose planning target volume and 40 Gy to the high-dose planning target volume in five fractions with three mm planning margins.
“For intra-fraction prostate motion, the real-time prostate displacements measured by ultrasound were exported for analysis,” according to Dr. Guo and her colleagues. “The percentage of time prostate movement exceeded a two mm threshold was calculated for each fraction of all patients. T-test was used for all statistical comparisons.”
Dr. Guo and her colleagues successfully used the transperineal ultrasound system on all 23 prostate SBRT patients and in 110 of the 115 treatment fractions for intra-fraction motion monitoring. “For the five fractions in which patients were treated without ultrasound monitoring, the probe remained in the same position as CT simulation to maintain the same anatomy.”
Data confirmed that the ultrasound image quality was sufficient for visualization of the prostate and surrounding organs at risk. The setup time for each fraction under ultrasound-guided prostate SBRT was 15.0 ± 4.9 minutes. The total treatment time per fraction was 31.8 ± 10.5 minutes.
“Our study not only demonstrates the feasibility of ultrasound-guided prostate SBRT, but also shows that it fits into our standard SBRT workflow,” says Dr. Guo. “The presence of an ultrasound probe did not compromise the contouring of targets or critical structures.”
The researchers monitored prostate intra-fraction motion throughout the entire treatment; however, they only analyzed motion after kilo-voltage cone beam computed tomography (KV-CBCT) and before the delivery completion.
Advertisement
A warning was triggered when prostate movements were more than 2 mm in any direction. This prompted clinicians to manually hold the beam until the prostate position returned back to within 2 mm threshold.
When discussing intro-fraction motion, Dr. Guo notes that prostate movement exceeded 2 mm tolerance in 23 of 110 fractions for 11 of 23 patients. “For all fractions, the mean percentage of time when the prostate moved more than 2 mm in any direction during each fraction was 7%, ranging from 0% to 62% of a fraction.”
Based on the researchers’ experience, the procedure was well-tolerated by patients. Additionally, the training for therapists is minimal and straightforward.
“This analysis suggests that ultrasound-guided prostate stereotactic body radiation therapy is an effective, non-invasive alternative for patients who cannot tolerate marker/spacer implantation or have other contraindications. The next step is to further simplify and streamline the process to benefit even more patients.”
Advertisement
Advertisement

An update on the technology from the busiest Gamma Knife center in the Americas

Approach offers a ‘middle ground’ between radical prostatectomy and active surveillance

AI histologic classifier reliably predicts clinical risk in men post-prostatectomy

Historic collaboration connects two Cleveland Clinic locations, enables real-time sharing of metrics and surgical progress

Radiation oncology department finds weekly plan of care meetings have multiple benefits

Daily five-fraction partial breast irradiation (PBI) shows similar acute and late toxicity as every other day PBI

Research highlights promising outcomes for treating recurrent and metastatic cases
Review the advantages and disadvantages of newer interventions