HALT has unique clinical implications for adults with congenital heart disease
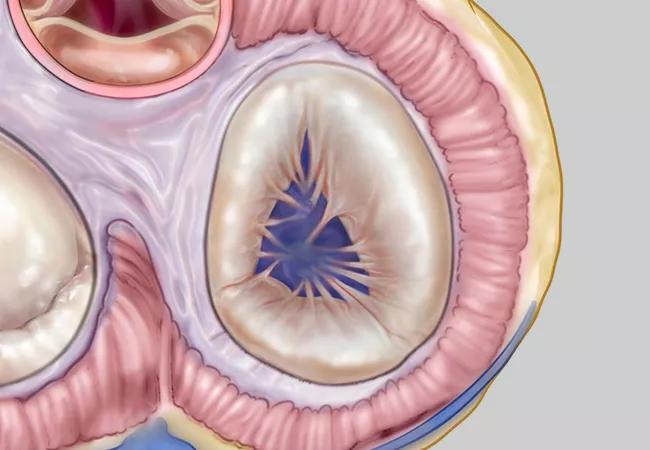
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/06606651-4ee7-42f9-8e5f-518030fe6e47/22-HVI-3413075_illustration-of-pulmonary-valve_650x450-jpg)
Pulmonary valve
Transcatheter pulmonary valve replacement (TPVR) is the standard of care in managing right ventricular outflow tract dysfunction, particularly in the growing population of adults with congenital heart disease. However, as the use of TPVR expands, questions regarding valve durability and complications such as hypoattenuating leaflet thickening (HALT) and hypoattenuation affecting motion (HAM) have emerged.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
HALT and HAM have been studied mostly in transcatheter aortic valve replacement (TAVR), where they have been linked with increased risks of stroke, transient ischemic attacks and mortality, as well as valve deterioration. However, their implications in TPVR remain less understood.
A recent retrospective cohort study at Cleveland Clinic is the first to assess HALT and HAM in TPVR.
“There’s still a significant gap in our understanding of how these conditions manifest in adults with congenital heart disease undergoing TPVR,” says the study’s senior author, Joanna Ghobrial, MD, MSc, Medical and Interventional Director of Cleveland Clinic’s Adult Congenital Heart Disease Center. “Unlike patients with calcific aortic stenosis seen in TAVR, patients with TPVR are younger and face unique challenges, including the critical need for valve durability to minimize repeated interventions. This distinct patient population requires tailored approaches to managing bioprosthetic valve thrombosis.”
The study (JACC: Adv. 2025 Mar;4(3):101599) analyzed outcomes in 106 patients who had TPVR at Cleveland Clinic between 2018 and 2024. Of these, 46 patients had follow-up computed tomography angiography (CTA) to assess for HALT and HAM.
HALT was identified in 17.4% of patients (8 out of 46), and HAM was present in 6.5% (3 out of 46). These rates align with previously reported HALT and HAM prevalence in TAVR, which ranges from 10% to 30%.
Among patients with HALT, 37.5% (3 out of 8) demonstrated valve deterioration, characterized by increased valvular gradients or progression of regurgitation detectable by echocardiography. In contrast, the overall cohort had a much lower rate of valve deterioration (7.5%).
Advertisement
Notably, no HALT or HAM was observed in patients on oral anticoagulation, suggesting a potential protective role.
“This study highlights the need for heightened clinical awareness of HALT and HAM in TPVR patients,” says study co-author Hani Najm, MD, Chair of Pediatric and Adult Congenital Heart Surgery at Cleveland Clinic. “While these phenomena may not always lead to immediate clinical consequences, their association with valve deterioration underscores the critical need for early detection and targeted management.”
Unlike the older population typically undergoing TAVR for calcific aortic stenosis, patients with TPVR are predominantly younger individuals with complex congenital heart disease. Many have undergone multiple prior surgeries, and their right ventricles have often endured years of volume or pressure overload.
“Valve durability is paramount, as these patients are at higher risk for repeated interventions over their lifetime,” Dr. Ghobrial says. “HALT and HAM could have more significant clinical consequences in this group, given their long-term reliance on prosthetic valves.”
Additionally, the lower pressure system of the pulmonary circulation may influence thrombosis risk differently than the systemic circulation in TAVR. While HALT in TAVR has been associated with cerebrovascular events, no pulmonary emboli were identified in this study’s TPVR patients. However, the CT scans were not specifically designed to detect distal pulmonary emboli, leaving this question open for future investigation.
Advertisement
The study’s findings could have several important clinical implications:
Other questions for future research include:
Dr. Najm notes, “This study is an important first step in understanding HALT and HAM in TPVR patients. However, larger, multicenter studies are needed to refine our understanding of these phenomena and develop evidence-based management protocols.”
Advertisement
By raising awareness of HALT and HAM in TPVR, this study highlights the need for tailored approaches to antithrombotic therapy, imaging protocols and long-term monitoring in adult patients with congenital heart disease. With further research, clinicians can better ensure valve longevity and reduce the burden of repeat interventions in this vulnerable population.
Advertisement
Advertisement
Advanced transcatheter options have expanded patient candidacy
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
Experts advise thorough assessment of right ventricle and reinforcement of tricuspid valve
Reproducible technique uses native recipient tissue, avoiding risks of complex baffles
A reliable and reproducible alternative to conventional reimplantation and coronary unroofing
Retrospective study examines outcomes associated with common treatment pathways
Experts raise concerns, make recommendations about improving the data
Survival is improving, but the youngest patients still face disproportionate risk