IgA nephropathy is a relatively common autoimmune glomerular disease that can be diagnosed only by biopsy
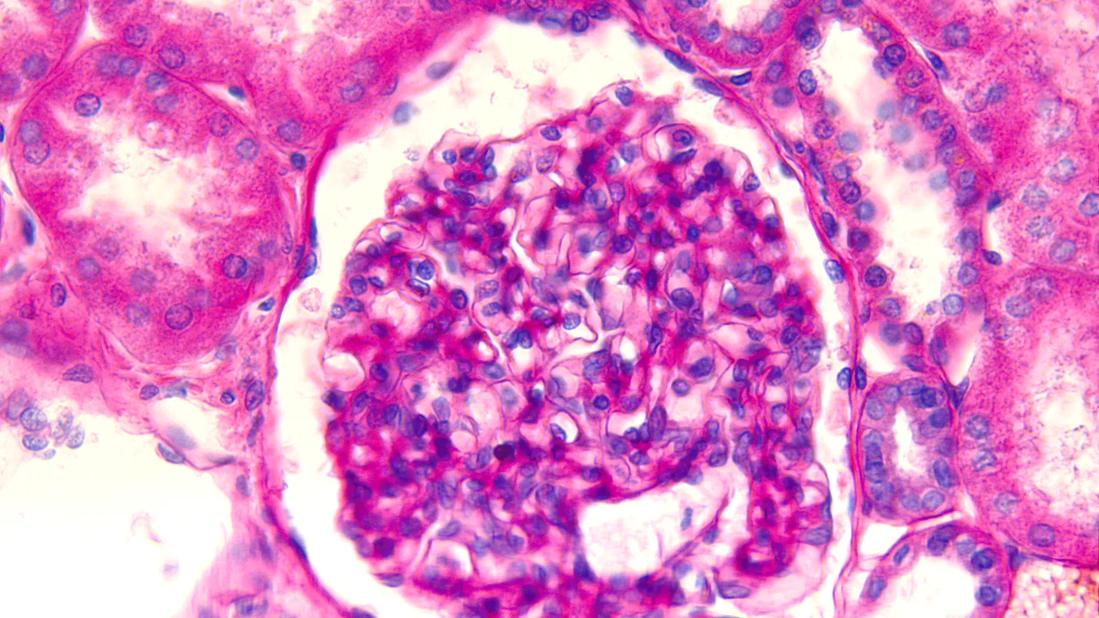
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/746f2c9c-b8b6-4c83-ad5c-765db8945d71/IgA-nephropathy-1182861877)
Pathology slide of IgA
By Seshma Ramsawak, MD, Scott Cohen, MD, Andrea Linares, DO and Corey Cavanaugh, DO
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Editor’s note: This article is reprinted from the Cleveland Clinic Journal of Medicine. It is the first section of a two-part series and highlights new updates and evidence relating to the pathogenesis of immunoglobulin (Ig) A nephropathy as well as diagnostic and prognostic tools. Part 2 focuses on current treatment options and those under investigation. The article in its entirety, including a full list of references, can be found here.
A major cause of kidney failure in children and adults, immunoglobulin (Ig) A nephropathy is the most common primary glomerulonephritis; its worldwide incidence is at least 2.5 per 100,000.
Opportunities for new therapies stem from the acknowledgment by the US Food and Drug Administration (FDA) that proteinuria reduction is an acceptable trial end point in the path to drug approval. This recent innovation is also a direct consequence of years of basic science research that has refined our understanding of the pathogenesis of IgA nephropathy into a framework of “four hits,” with each hit representing a target of novel therapies.
IgA nephropathy is an autoimmune disease of mucosal type IgA characterized by deposition of immune complexes in the glomerulus. Its pathogenesis is now firmly established and understood as the four-hit hypothesis (Figure 1). The four hits comprise a complex interplay of genetic factors (involving polymorphisms in human leukocyte antigen, complement and gut mucosal immunity) and environmental factors such as the gut microbiome, all of which contribute to the development of IgA nephropathy.
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/073a080b-c74a-4530-8bd8-af084f367161/IgA-nephropathy-figure1)
Figure 1. Pathogenesis of immunoglobulin (Ig) A nephropathy: the “4-hits” hypothesis.
Hit 1: Excessive production of galactose-deficient IgA1
Galactose-deficient IgA1 in IgA nephropathy lacks the terminal galactose moieties at the hinge region of the molecule. The primary site for production of galactose-deficient IgA1 is now believed to be the gut and nasal mucosa. Many factors have been implicated in the production of galactose-deficient IgA1.
Genetics may influence the O-galactosylation of the IgA hinge region. Abnormal galactosylation of IgA can be an inherited trait, but this alone is insufficient for development of IgA nephropathy.
Cytokines, including serum B-cell activating factor (BAFF) and a proliferation-inducing ligand (APRIL), are important regulators of mucosal B-cell survival and proliferation. BAFF and APRIL promote the formation of galactose-deficient IgA1–producing plasma cells in the mucosa.
Alterations in the composition of the gut micro-biome (which communicates with mucosal-associated lymphoid tissue) have been implicated in IgA nephropathy. Mucosal dysbiosis may be related to dysregulated mucosal IgA synthesis. Recently, it was shown that patients with IgA nephropathy have a relative overgrowth of mucin-degrading bacteria, which are capable of deglycosylating IgA1.
Hit 2: Production of autoantibodies to galactose-deficient-IgA1
Antibodies, either IgG or IgA, recognize the galactose-deficient hinge region of galactose-deficient IgA1, a neoepitope. Routine immunofluorescence on kidney biopsy detects IgA bound to galactose-deficient IgA1 as the predominant immune complex deposited; however, evidence supports the presence of IgG autoantibodies, which also play a role in the pathogenesis of the disease.
Advertisement
Hit 3: Formation of immune complexes consisting of IgG autoantibodies bound to galactose-deficient IgA1
Clinical and histologic activity correlate with the level of circulating immune complexes. Additionally, alternative complement and terminal complement activity have been shown to correlate with the concentration of galactose-deficient IgA1.
Hit 4: Deposition of immune complexes into the glomerulus
The effect of the immune complexes on mesangial cells within the glomerulus drives kidney injury. Deposition of immune complexes activates mesangial cells, leading to production of inflammatory molecules such as interleukin-6 and platelet-derived growth factor and complement, which signal infiltration of monocytes and mediate glomerular injury.
Complement plays a prominent role in mesangial injury and is a major driver of glomerular inflammation. C3 is deposited in the mesangium, activating both the alternative and lectin pathways. In vitro studies provide evidence of alternative pathway proteins such as complement components C5, C6, and C9 and other membrane attack complex antigens in the glomeruli of patients with IgA nephropathy, whereas markers for classical pathway activation such as C1q and C4 are less prominent. Complement factor H–related protein competes with the binding of factor H, a regulator protein, leading to an increase in the activity of the alternate complement pathway.
Despite advances in understanding the pathogenesis of IgA nephropathy, diagnosis requires a kidney biopsy. Clinical suspicion arises from the presence of acute kidney injury, hematuria, or proteinuria. Uncommonly, patients present with gross hematuria or synpharyngitic hematuria (hematuria with pharyngitis), a presentation seen more often in younger patients (< 40 years). In older populations, IgA nephropathy can be clinically occult with worsening kidney function and microscopic hematuria. While routine screening is common in countries with a high prevalence, such as Japan and China, there are no screening guidelines in the United States. Therefore, timely referral to nephrology upon discovery of hematuria or proteinuria is critical.
Advertisement
Histologic examination of the kidney biopsy specimen with immunofluorescence microscopy will show IgA deposits in the mesangium or capillary loops accompanied by mesangial changes (proliferation and expansion). Serologic markers, while extensively studied and now frequently used in clinical trials, require further validation before they can be applied in the clinic.
Alternative diagnoses must be considered when histopathology reveals IgA staining, as there are numerous mimics of primary IgA nephropathy (Table 1). Systemic disease states associated with IgA nephropathy, labeled secondary IgA nephropathy, include IgA vasculitis, viral infections (human immunodeficiency virus, hepatitis), autoimmune disease (inflammatory bowel disease, psoriasis), cirrhosis, IgA-dominant postinfectious glomerulonephritis and proliferative glomerulonephritis with monoclonal IgA deposits.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/70e338d5-97f1-49cb-940f-890a2f6c1001/IgA-nephropathy-table1)
Table 1. Immunoglobulin (Ig) A nephropathy and its mimics
Once the diagnosis is established, the characteristic findings are used to determine prognosis and clinical outcomes. Secondary IgA nephropathy and IgA vasculitis have been largely excluded from clinical trials and carry a different prognosis than primary IgA nephropathy.
Oxford Classification of IgA nephropathy was introduced in 2009. The purpose was to create a standardized histopathologic scoring system using four variables that correlate most strongly with patient outcomes, in addition to showing adequate agreement among nephropathologists. The variables are mesangial hypercellularity (M), endocapillary hypercellularity (E), segmental glomerulosclerosis (S), and tubular atrophy/interstitial fibrosis (T), reported as the MEST score. The system was updated in 2016 to incorporate crescents (C) to further aid in predicting renal outcomes (Table 2).
Advertisement

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d0ef8064-e63c-468d-ad61-585084116ec7/IgA-nephropathy-table2)
Table 2. Oxford classification of immunoglobulin A nephropathy: MEST-C score
M, S and T were found to be independent predictors of glomerular filtration rate (GFR) decline in the original Oxford cohort, but E lesions were not conclusively predictive of decline. Similar associations in GFR decline were seen in patients with endocapillary hypercellularity (E) independent of immuno-suppression. The Oxford cohort did not control for immunosuppression, leading to a treatment bias. Further, patients with E lesions were more likely to receive immunosuppression. Collectively, this evidence supports the perception that endocapillary lesions are responsive to immunosuppressive treatment and contribute to the decline of kidney function if not treated with immunosuppression.
Although helpful for diagnostic standardization and prognosis, this scoring system does not consider the presence of hypertension, degree of proteinuria, or reduced GFR.
The introduction of the international IgA nephropathy risk prediction tool further refines risk stratification by integrating histologic and clinical factors to predict renal outcomes at the time of biopsy and up to seven years. It was derived in a multiethnic international cohort with biopsy-proven idiopathic IgA nephropathy and is designed to predict the risk of a 50% decline in estimated GFR or end-stage kidney disease after biopsy.
This web-based prediction tool includes the estimated GFR at the time of biopsy, systolic and diastolic blood pressure at the time of biopsy, proteinuria, age, race, use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, MEST score, immunosuppression use at or before kidney biopsy, and the number of months after a kidney biopsy that the clinician will determine the risk of progressive IgA nephropathy.
Criticisms of the IgA nephropathy prediction tool include its lack of dynamic longitudinal monitoring ability and the absence of modern therapies (endothelin receptor antagonists and sodium-glucose cotransporter [SGLT] 2 inhibitors). Also, it was not validated to guide the use of immunosuppression.
Part 2 of the two-part series unpacks current therapeutic options and those currently under investigation. The article in its entirety, including a full list of references, can be found here.
Dr. Ramsawak is a former Cleveland Clinic nephrology fellow, and Drs. Cohen, Linares and Cavanaugh are staff nephrologists.
Advertisement
Proteinuria reduction remains the most important treatment target.
Significant improvement in GCSI scores following treatment
Pediatric urologists lead quality improvement initiative, author systemwide guideline
Fixed-dose single-pill combinations and future therapies
Reproductive urologists publish a contemporary review to guide practice
Two recent cases show favorable pain and cosmesis outcomes
Meta-analysis assesses outcomes in adolescent age vs. mid-adulthood
Oncologic and functional outcomes are promising, but selection is key