Companion studies reveal efficacy indicators for PD-1/PD-L1 inhibition
Patients with non-small cell lung cancer (NSCLC) brain metastases and a KRAS mutation — a genotype associated with an especially poor prognosis — who were treated with immune checkpoint inhibitors had a one-year survival rate equivalent to that of patients without the mutation in a large cohort study. This notable finding was reported by a team of Cleveland Clinic researchers in an oral presentation at the Society for Neuro-Oncology Inaugural Conference on Brain Metastases on Aug. 17 in New York.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A second oral presentation from the Cleveland Clinic research team further defined clinical parameters of efficacy of immunotherapy for NSCLC brain metastases, demonstrating that upfront steroid therapy was associated with worsened outcomes and that a high neutrophil-to-lymphocyte ratio was associated with poor prognosis.
“Immunotherapy has brought about a dramatic change in medical treatment for non-small cell lung cancer, one of the deadliest cancers and the most common cause of brain metastases,” says neuro-oncologist Manmeet S. Ahluwalia, MD, Director of the Brain Metastasis Research Program at Cleveland Clinic’s Rose Ella Burkhardt Brain Tumor and Neuro-Oncology Center. “Our findings confirm the importance of immunotherapy in treating brain metastases and reveal critical indicators of efficacy.”
Dr. Ahluwalia was the senior investigator for both studies, which drew from a database of 1,000 patients treated at Cleveland Clinic for NSCLC brain metastases between 2012 and 2018. He also served as scientific program co-chair of the conference.
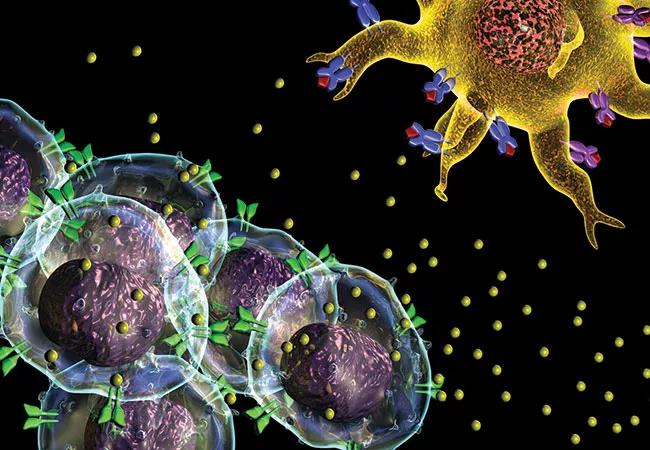
So-called checkpoints are molecules (referred to as “PD-1”) on T cells that can be activated by ligands (referred to as “PD-L1”) presented by other cells to limit an immune response. This is especially important under normal circumstances to minimize the killing of host cells and prevent autoimmune disease. Cancer cells may take advantage of PD-1 checkpoints by activating them themselves, thereby dampening the host immune system and avoiding attack. To this end, some cancer cells express many PD-L1 proteins.
Advertisement
Immune checkpoint inhibitors (ICIs) include monoclonal antibodies that target PD-1 (pembrolizumab, nivolumab) or PD-L1 (atezolizumab) molecules to block cellular protein binding, with the effect of boosting the host immune response.
Of the 1,000 patients in the Cleveland Clinic database, 226 had known KRAS mutational status; 121 of them received at least two cycles of immunotherapy. The KRAS gene acts as an on-off switch to control cell proliferation; KRAS mutations disrupt negative signaling, causing cells to continuously proliferate by recruiting and activating proteins necessary for growth.
The first study from this database examined overall survival according to whether patients had a KRAS mutation or wild-type KRAS and whether or not they received immunotherapy. “Patients with KRAS mutations usually fare worse than patients with wild-type KRAS when treated with chemotherapy, after adjusting for age, Karnofsky Performance Status, lesion number and extracranial metastasis,” Dr. Ahluwalia notes.
Findings of the study, which assessed survival from the start of immunotherapy or the date brain metastasis was diagnosed, included the following.
Advertisement
The greater benefit with immunotherapy relative to chemotherapy in patients with KRAS mutations may be explained by the fact that these patients were more likely to test positive for PD-L1 expression than were patients with wild-type KRAS (80.1% vs. 61.9%, P = 0.04). Both KRAS and PD-L1 status were known for 109 patients.
“Greater expression of PD-L1 — the target of ICI therapy — sets the stage for immunotherapy to be highly effective,” explains Dr. Ahluwalia. “It actually brings the notoriously poor survival rates associated with KRAS mutations up to the level achieved in wild-type KRAS patients.”
The second study examined characteristics and outcomes among the 121 patients who received ICI therapy, whose profile was as follows:
Evaluation of progression-free and overall survival rates revealed two significant trends. Worse outcomes were seen with:
Advertisement
“Steroids are immunosuppressive, so it’s not surprising that they reduce the effectiveness of immune-enhancing ICI therapy,” notes Dr. Ahluwalia.
Regarding the NLR findings, he adds: “Although NLR provides prognostic information, we don’t know whether it impacts the efficacy of therapy or is merely a marker of overall health.”
Dr. Ahluwalia says two main conclusions can be drawn from this research:
1) For a patient with NSCLC brain metastasis who has a KRAS mutation, immunotherapy is indicated.
2) For patients on immunotherapy who need steroids, minimizing the steroid dose is important.
His research group is now assessing different combinations of therapeutic approaches, such as immunotherapy with radiosurgery, to evaluate efficacy and focus on strategies for reducing steroid use in patients treated with immunotherapy.
Advertisement
Advertisement

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists