Results of the largest population-based study to date
Inflammatory bowel disease (IBD) patients treated with biologics are significantly less likely to have osteoporosis and bone fractures compared with those who did not, according to the largest individual study to date investigating the prevalence of osteoporosis and bone fractures in IBD patients with and without biologics therapy.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
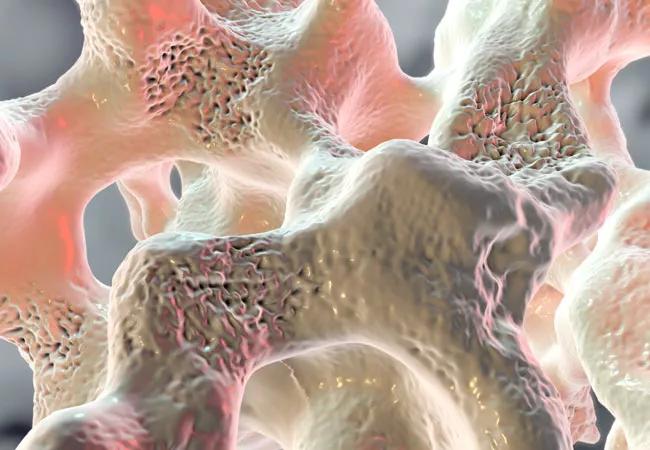
“We know that IBD patients tend to exhibit a higher risk of developing bone loss compared with the general population,” notes study author Ahmed Eltelbany, MD, MPH, staff in the Department of Hospital Medicine at Cleveland Clinic. “It is also well-known that IBD patients are in a state of chronic inflammation that causes a reduction in bone mineral density, which can lead to osteopenia, osteoporosis and pathological bone fractures.”
Biologics have shown to decrease inflammation among this patient population, according to Dr. Eltelbany. “While previous studies suggest that biologics may reduce osteoporosis, this has not been shown in a larger population-based study, which prompted us to initiate our research.”
The study utilized a commercial database, which includes electronic health record data from 26 major integrated U.S. healthcare systems, to identify all patients (age 18 years or older) who were diagnosed with either Crohn’s disease or ulcerative colitis between 2015 and 2020 and treated with any type of biologics.
Researchers investigated the prevalence of osteoporosis and bone fractures in IBD patients compared with patients with no IBD. They also compared the prevalence between IBD patients with and without biologics therapy.
Of the 31,040,480 individuals in the database, Dr. Eltelbany and colleagues identified 135,630 (0.44%) patients with Crohn’s disease and 112,060 (0.36%) with ulcerative colitis, of whom 26,140 (19.3%) and 9,370 (8.4%) received biologics therapy, respectively.
Advertisement
Data revealed that the prevalence of osteoporosis and bone fractures was 8.3% and 8.9% for Crohn’s disease and 7.4% and 8.7% for ulcerative colitis, compared with 3.7% and 9.0%, respectively, among individuals without IBD.
The researchers found that the prevalence of osteoporosis and bone fractures was significantly lower among Crohn’s disease patients treated with biologics (7.3% and 6.8%) compared with those who did not receive biologics (12.7% and 14.6%).
Similarly, patients with ulcerative colitis who received biologics were significantly less likely to have osteoporosis and bone fractures (5.9% and 5.5%) compared with ulcerative colitis patients who had not received this treatment (11% and 14.9%).
The data also showed that 94% of Crohn’s disease patients and 96% of ulcerative colitis patients who underwent biologics therapy previously received corticosteroids — an established risk factor for osteoporosis. This is an interesting finding, according to Dr. Eltelbany, which suggests that the benefits for resistance in the biologics-treated cohort remains despite receiving steroids.
“We know that patients with inflammatory bowel disease have a higher prevalence of osteopenia, osteoporosis and consequent bone fractures. This can lead to considerable morbidity,” reiterates Miguel Regueiro, MD, Chair of the Digestive Disease & Surgery Institute at Cleveland Clinic, while noting that the reason for bone thinning is probably multifactorial. Potential causes include malabsorption of vitamin D and calcium, the use of corticosteroids and possibly the active gut inflammation.
Advertisement
“The theory that active IBD itself leads to osteoporosis is of great interest,” he continues. “We think that the active immune chemicals, e.g., cytokines such as TNF alpha, may actually promote bone loss. To that end, the use of biologics may actually lessen the systemic cytokines and prevent bone loss.
“In our nationwide study we found that the use of biologics seems to reduce the prevalence of osteoporosis,” Dr. Regueiro concludes. “The implication of this is important as this study supports the active treatment of IBD to improve gut health and potentially reduce the risk of osteoporosis and bone fractures.”
The study authors note that the next steps include randomized controlled trials that explore the impact of biologics on bone marrow density and osteoporosis. This will provide a deeper understanding of the benefits of biologics for these patients as well as help determine whether the duration of treatment positively correlates with the reduction of osteoporosis.
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications