Insights from the STAMPEDE trial compare outcomes after metabolic surgery versus medical therapy
Individuals who undergo metabolic surgery for their diabetes and obesity experience improved quality of life (QoL), physical functioning, and general health perceptions compared with those who were treated with medications and lifestyle modification according to a new study from Cleveland Clinic researchers that appeared in Annals of Surgery. The findings are from a follow-up study on the Surgical Treatment and Medications Potentially Eradicate Diabetes Efficiently (STAMPEDE) randomized clinical trial.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
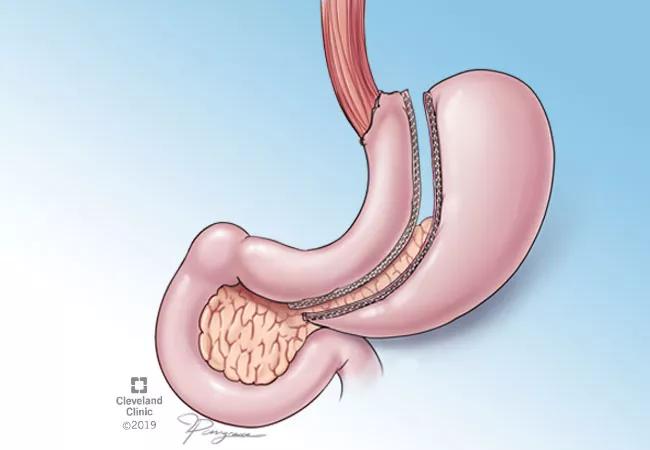
The present study examined the long-term effects of medical and surgical treatments of T2DM on patient reported outcomes (PROs). The STAMPEDE trial found that five years after randomization, Roux-en-Y gastric bypass (RYGB) and sleeve gastrectomy (SG) were both superior to intensive medical therapy (IMT) alone in achieving diabetes remission in patients with T2DM and obesity.
From March 2007 to January 2011, 150 of patients with T2DM and obesity were randomized into three groups: IMT alone or IMT plus either laparoscopic RYGB or SG. Among them, researchers examined PROs data from 104 patients who completed two standardized QoL questionnaires (RAND-36 and EQ-5D-3L). Participants also completed a diabetes-specific survey at baseline and annually up to five years after randomization.
The authors found that the baseline characteristics were similar among the three cohorts. However, five years after randomization, patients’ self-reported QoL outcomes were significantly improved in those who received metabolic surgery with respect to body pain, energy/fatigue, physical functioning, and general health perceptions compared with those who were only treated with medications and lifestyle modification.
“Factors related to improved QoL were related to weight loss and insulin independence achieved by patients who underwent metabolic surgery,” says Ali Aminian, MD, the Director of Bariatric and Metabolic Institute at the Cleveland Clinic and lead author of the study. “We found that metabolic surgery has long-term favorable changes in certain PROs compared with the IMT in patients with T2DM and moderate obesity, but this was primarily in physical health and diabetes-related domains.”
Patients with long duration of diabetes tend to have poor QoL, especially when they develop microvascular complications like eye and kidney diseases. “When diabetes is coupled with obesity, the impact on lower QoL is primarily related to the mechanical effects of obesity which lead to poor mobility and bodily pain,” explains Sangeeta Kashyap, MD, a physician scientist in the Endocrinology & Metabolism Institute at Cleveland Clinic and one of the study’s authors.
There were a few limitations to the study. Patients screened for metabolic surgery were assessed for psychological disorders, but those screened for IMT were not. Patients in the study were majority women (66%) and white (73%), so caution should be used when applying these results to other populations. There was also a lack of annual PRO data for some patients, which resulted in enrollment of only 106 patients in three groups, which may contribute in inability to identifying statistical differences in some study outcomes.
“There are several benefits to large weight loss, including reduced pressure on joints, decreased musculoskeletal pain, and improved mobility. Our findings show that improved diabetes control and taking less medications — particularly injectables — may also contribute to a patient’s satisfaction after metabolic surgery,” says Dr. Kashyap.
Incidence, outcomes and management

Cleveland Clinic endocrinologists work to identify protocols for improving care
Cleveland Clinic’s Endocrinology & Metabolism Institute is working to offer novel opportunities and therapies for diabetes and kidney disease

New findings indicate the importance of achieving sufficient sleep levels in regard to personal glucose targets
A recent study evaluates the correlation between preoperative calcium and parathyroid hormone values as predictors of gland volume and multi-gland disease

A look at how to asses hCG elevation

As the diet’s popularity rises, certain considerations need to be taken when recommending it for patients with Type 1 diabetes

Findings suggest that the effectiveness of interventions may depend more on the frequency and delivery methods of the intervention rather than who is delivering the intervention