Sorting out pros and cons of various imaging studies
By Bo Xu, MBBS (Hons); Paul Cremer, MD; Wael Jaber, MD; Stuart Moir, MBBS, PhD; Serge C. Harb, MD; and L. Leonardo Rodriguez, MD
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 62-year-old woman with hypertension and type 2 diabetes mellitus has been experiencing shortness of breath on exertion and chest discomfort for two months. Her hypertension has been suboptimally controlled, and her most recent hemoglobin A1c measurement was 7.0 percent. She has never smoked and has no family history of premature coronary artery disease (CAD). She is otherwise well and walks for 30 minutes three times per week. A 12-lead ECG demonstrated normal sinus rhythm with left bundle branch block. Her physician suspects she has CAD. What testing does this patient need?
For clinicians investigating suspected obstructive CAD in patients with left bundle branch block on resting ECG, the data and guidelines are limited regarding the optimal noninvasive tests and how to interpret them.
We present here a practical review of the diagnostic utility of exercise stress ECG , exercise stress echocardiography, dobutamine stress echocardiography, nuclear myocardial perfusion imaging, and CT angiography for assessing suspected obstructive CAD in patients with resting left bundle branch block.
In left bundle branch block, as the name implies, electrical conduction along the left bundle branch is blocked or delayed. Ventricular activation therefore begins in the right ventricle and the right side of the interventricular septum.1 Transseptal activation from the right ventricle to the left ventricle is slow, because it is transmyocardial.1 Left ventricular basal and posterolateral wall segments become activated last.1 Due to delay in the onset of left ventricular contraction, ventricular contraction is dyssynchronous. Classically, interventricular septal motion during systole has been described as paradoxical, with anterior septal motion.2-4
On ECG, the QRS duration is widened (≥ 120 ms), with a distinctive morphology as shown in Figure 1. Left bundle branch block makes it difficult to accurately assess for dynamic ST-segment changes with exercise, rendering exercise stress ECG a suboptimal test for obstructive CAD if left bundle branch block is present.
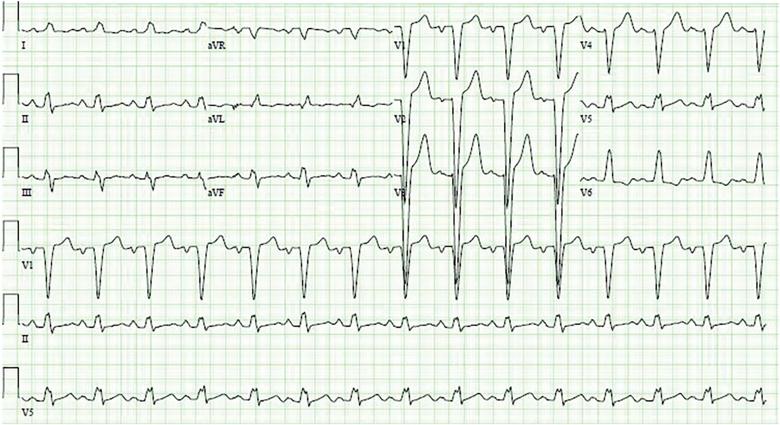
Figure 1. A 12-lead ECG from a 70-year-old woman with a 12-month history of progressive exertional dyspnea demonstrates sinus rhythm with a ventricular rate of 88 beats per minute and a wide left bundle branch block (QRS duration 150 ms).
Although left bundle branch block can be an isolated finding, it can also be associated with underlying obstructive CAD5 or cardiomyopathy.6 When it occurs at rest, the risk of death from a cardiovascular event is three to four times higher.7 However, the exact incidence of significant obstructive CAD in asymptomatic patients with incidentally detected left bundle branch block is unknown.
Acute left bundle branch block accompanying acute myocardial infarction is associated with a high risk of death. Hindman et al,8 in a 1978 multicenter study, described 432 patients with acute myocardial infarction and left or right bundle branch block. In the 163 patients who had left bundle branch block, the in-hospital mortality rate was 24 percent and the one-year mortality rate was 32 percent.
Freedman et al9 in 1987 reviewed 15,609 patients with chronic CAD who underwent coronary angiography, of whom 522 had left or right bundle branch block. During a follow-up of nearly five years, 2,386 patients died. The actuarial probability of death at two years in patients with left bundle branch block was more than five times that of patients without it (P < .0001).
During 18 years of observation in the Framingham study,10 55 participants developed left bundle branch block, at a mean age of 62. Twenty-six (48 percent) of these participants developed clinically significant CAD or heart failure coincident with or subsequent to the onset of left bundle branch block. Fifty percent of the participants who developed left bundle branch block died of cardiovascular disease within 10 years of its onset.
Exercise stress ECG, although valuable for assessing functional capacity, cannot be used to diagnose obstructive CAD in patients with left bundle branch block.11
Exercise stress echocardiography is proven and widely used for assessing myocardial ischemia in patients with suspected obstructive CAD. But the data are limited on its diagnostic utility in patients with left bundle branch block. Until recently, recommendations for its use in this situation were based on only one small study.12
In that study, published in 2000, Peteiro et al12 described 35 patients who underwent exercise stress echocardiography and coronary angiography. Detection of wall-motion abnormalities had high sensitivity (76 percent), specificity (83 percent) and diagnostic accuracy (80 percent).
Of note, 8 of the patients (23 percent) could not achieve at least 85 percent of the maximum predicted heart rate, and for them, the study was not diagnostic for ischemia. (Technically, the study is said to be nondiagnostic when the patient fails to achieve the target heart rate of at least 85 percent of the maximum predicted heart rate.)
Additionally, 18 of the 35 patients — over half — had a decrease in left ventricular ejection fraction in response to exercise. These 18 patients included 12 of the 17 patients with obstructive CAD and 6 of the 18 patients without obstructive CAD.12 It is unclear whether a significant proportion of these 18 patients would have been otherwise categorized as having a globally abnormal left ventricular contractile response to exercise according to contemporary (2007) reporting standards.13
More recently (2016), Xu et al14,15 examined the diagnostic utility of exercise stress echocardiography in assessing suspected obstructive CAD in 191 patients with resting left bundle branch block; 17 patients who failed to achieve a heart rate of at least 85 percent of the age-predicted maximum heart rate were excluded. Of the remaining 174 patients, 82 demonstrated a normal left ventricular contractile response to exercise and 92 had an abnormal response. In the abnormal group, 70 patients had a globally abnormal response and 22 had a regional ischemic response. Of those who had a globally abnormal left ventricular contractile response who subsequently underwent angiography, only 30 percent were found to have obstructive CAD.
Although the sensitivity of exercise stress echocardiography was high (94 percent), its specificity and diagnostic accuracy were poor (specificity 21 percent, diagnostic accuracy 52 percent).14,15 These results suggest that for patients with resting left bundle branch block undergoing exercise stress echocardiography, obstructive CAD cannot be reliably diagnosed in those who develop a globally abnormal left ventricular contractile response. Therefore, an alternative imaging strategy should be considered.
The evidence base for dobutamine stress echocardiography in patients with left bundle branch block is more robust than that for exercise stress echocardiography.
Geleijnse et al1 studied 64 patients with left bundle branch block undergoing dobutamine stress echocardiography who also underwent coronary angiography. Dobutamine stress echocardiography was moderately sensitive for detecting anterior and posterior myocardial wall ischemia (60 percent and 67 percent, respectively). Its specificity and diagnostic accuracy were high, at 94 percent and 98 percent, respectively.
Yanik et al16 studied 30 patients with left bundle branch block undergoing both dobutamine stress echocardiography and coronary angiography. The sensitivity of dobutamine stress echocardiography for identifying ischemia in the left anterior descending territory was 82 percent, the specificity was 95 percent and the diagnostic accuracy was 90 percent. For identifying ischemia in the circumflex and right coronary artery territories, sensitivity was 88 percent, specificity 96 percent and accuracy 93 percent.
Mairesse et al17 studied 24 patients with left bundle branch block undergoing dobutamine stress echocardiography, myocardial perfusion tomography, and coronary angiography. Dobutamine stress echocardiography performed well in detecting ischemia in the left anterior descending territory, with a sensitivity of 83 percent, specificity of 92 percent and diagnostic accuracy of 87 percent.
Of note, the available data come from very small studies published more than 15 years ago, and pharmacologic stress testing cannot provide the very important prognostic information derived from treadmill testing.
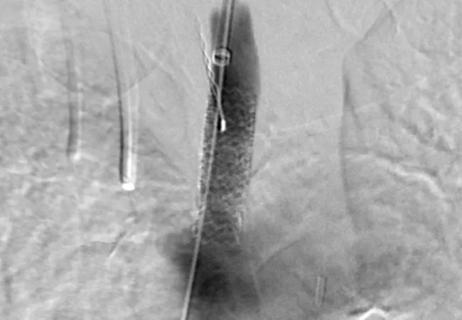
Exercise nuclear single-photon emission computed tomography (SPECT) myocardial perfusion imaging in patients with left bundle branch block is challenging, due to the development of septal perfusion defects at rest and during exercise in the absence of obstructive disease in the left anterior descending artery (Figure 2).18,19 Possible explanations for this phenomenon are asynchronous contraction of the septum, with resulting compression of the septal arteries, decreased flow demands to the septal region and attenuation artifacts.20
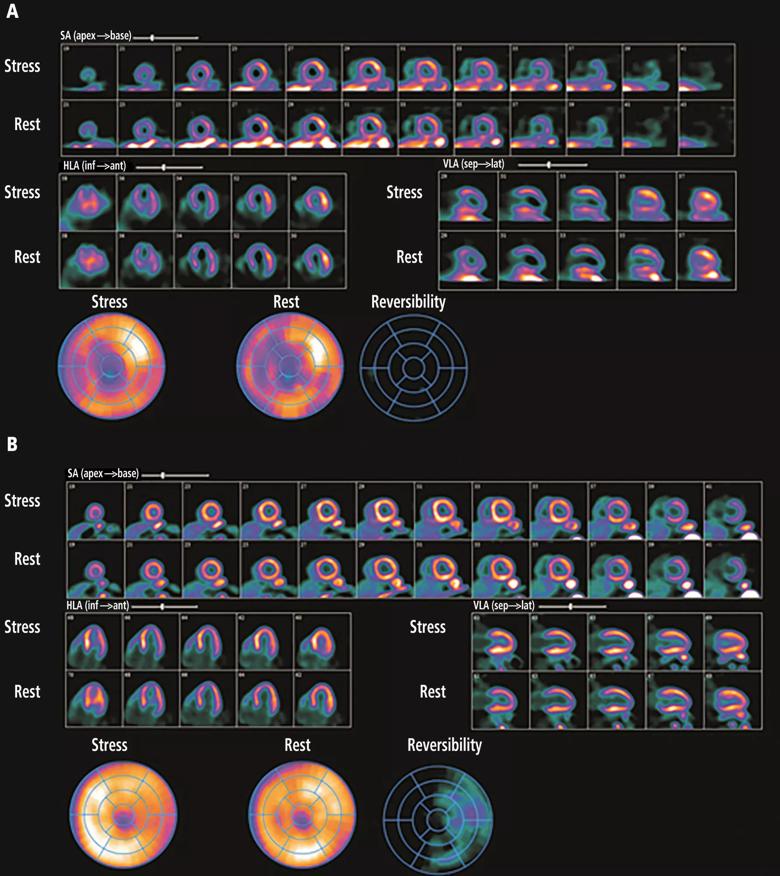
Figure 2. Pharmacologic nuclear myocardial perfusion imaging in a 75-year-old woman with atypical symptoms and resting left bundle branch block on ECG. (A) Fixed perfusion defects were present at rest and after pharmacologic stress with regadenoson in the septum and apex on single-photon emission computed tomography, mimicking ischemic damage in the left anterior descending artery territory. (B) In comparison, on positron emission tomography, no perfusion abnormalities were seen at rest or with regadenoson.
Pharmacologic stress has been reported to improve the diagnostic accuracy of SPECT myocardial perfusion imaging. Biagini et al,21 in a meta-analysis of noninvasive techniques for diagnosing CAD in patients with left bundle branch block, found 1,785 patients from 39 studies who underwent nuclear myocardial perfusion imaging (48.8 percent with exercise, 41.9 percent with pharmacologic stress). Overall, sensitivity was high for both exercise and pharmacologic stress (92.9 percent and 88.5 percent). However, the reported specificity with exercise stress was significantly lower than with pharmacologic stress (23.3 percent vs. 74.2 percent; P < .01).
Nuclear positron emission tomography (PET) may further improve the diagnostic utility of nuclear myocardial perfusion imaging in patients with left bundle branch block. In a study of 440 patients with left bundle branch block undergoing myocardial perfusion imaging, 67 underwent PET and 373 underwent SPECT.22 Possible septal perfusion artifacts were significantly less common with PET than with SPECT (1.5 percent vs 19.3 percent; P < .001).
CT angiography has high sensitivity and specificity for detecting significant obstructive CAD.23,24 Machines with 320 detector rows have been reported to have a sensitivity of 94 percent and a specificity of 87 percent for detecting significant CAD and are not affected by resting left bundle branch block.25
Of note, coronary artery calcification increases in older patients, especially those age 65 and older,26 and this confers a higher likelihood of “bystander” CAD. Significant coronary artery calcification limits the diagnostic accuracy of multidetector cardiac CT. Additionally, the detection of bystander CAD leads to positive findings of uncertain clinical significance.
Exercise stress echocardiography. American College of Cardiology Foundation/American Heart Association guidelines for diagnosis and management of patients with stable ischemic heart disease recommend exercise stress echocardiography for patients with an intermediate to high pretest probability of ischemic heart disease who have an uninterpretable ECG and at least moderate physical functioning or no disabling comorbidity (class 1 indication, level of evidence B).11
Current American Society of Echocardiography guidelines also support exercise stress echocardiography as an appropriate test for suspected obstructive CAD in patients with resting left bundle branch block.27 However, this recommendation is based on limited data.
Pharmacologic stress nuclear myocardial perfusion imaging.American Society of Nuclear Cardiology guidelines endorse pharmacologic stress nuclear myocardial perfusion imaging using coronary vasodilators for evaluating suspected obstructive CAD in patients with resting left bundle branch block.28,29
Although current guidelines recommend it, recent data show that exercise stress echocardiography has poor specificity and diagnostic accuracy for significant obstructive CAD in patients with resting left bundle branch block. And performing this test in patients with left bundle branch block may result in further downstream investigations.
Based on limited data from a small number of studies published more than 15 years ago, dobutamine stress echocardiography has moderate sensitivity and specificity for significant CAD in patients with resting left bundle branch block. However, this test does not provide functional information about the patient’s exercise performance.
Pharmacologic stress nuclear myocardial perfusion imaging using coronary vasodilators is an appropriate investigation strategy. However, radiation exposure is a limitation.30
CT angiography can assess for significant obstructive CAD in patients with resting left bundle branch block. However, its diagnostic accuracy can be affected by coronary calcification in older patients. Additionally, each scan is associated with a small amount of radiation exposure,31 and a small number of patients will have a true contrast allergy.32
For patients with typical ischemic symptoms and new left bundle branch block on ECG, specialist cardiology consultation should be sought, with consideration given to proceeding directly to coronary angiography. For stable outpatients, we propose the following diagnostic approach (Figure 3).
Exercise stress echocardiography is recommended by current guidelines, but it cannot reliably detect significant obstructive CAD in patients with resting left bundle branch block, as its specificity and diagnostic accuracy are poor.14,15 Alternative imaging strategies include CT angiography, pharmacologic nuclear myocardial perfusion imaging using coronary vasodilators, and dobutamine stress echocardiography.
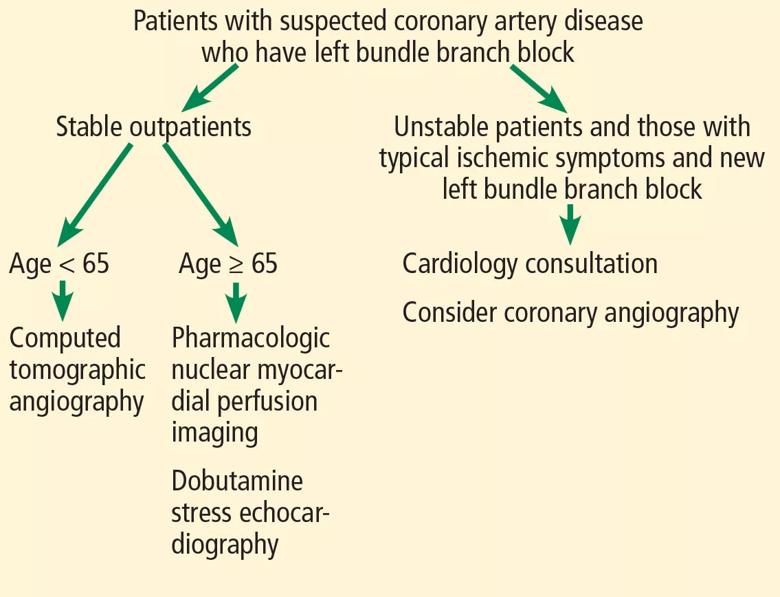
Figure 3. Proposed diagnostic pathway for patients with suspected obstructive coronary artery disease and resting left bundle branch block.
For investigating suspected obstructive CAD in patients with resting left bundle branch block, we propose CT angiography as the first-line imaging test for patients under age 65 and pharmacologic stress nuclear myocardial perfusion imaging using coronary vasodilators or dobutamine stress echocardiography for those age 65 or older. For patients who cannot tolerate contrast due to renal impairment or who have a true contrast allergy, pharmacologic nuclear myocardial perfusion imaging using coronary vasodilators and dobutamine stress echocardiography may be used as alternatives.
This article originally appeared in the March 2018 issue of Cleveland Clinic Journal of Medicine (2018;85:224-230).
Drs. Xu, Cremer, Jaber, Harb and Rodriguez are with Cleveland Clinic’s Department of Cardiovascular Medicine. Dr. Moir is with MonashHeart, Monash Medical Centre, Clayton, Victoria, Australia.
How our first century has impacted cardiovascular practice

Review offers comprehensive assessment of the landscape for wearables and more

Preserving trust in research requires vigilance and consensus around statistical nuances

Cardiac surgeon Patrick Vargo, MD, reflects on his first year as Cleveland Clinic staff

Improved risk prediction for patients is at the heart of Dr. Aaron Weiss’ research interests

Centralization would likely bring better outcomes, experts say, but may not be feasible
Dr. Daniel Burns on mentorship, robotic valve surgery, statistics and more
JACC review makes the case and outlines how to ensure oversight