Can genomic classifiers contemporize stratification?
A clinically validated genomic classifier is associated with adverse histopathologic features of prostate cancer, including cribriform (CF) and intraductal carcinoma (IDC), according to a Cleveland Clinic-led study recently published in European Urology Focus. Small studies have hinted toward a role for genomic classifiers in risk stratification for prostate cancer, but this study, the largest series to date, suggests that genomic classifiers like the Decipher test can improve individual risk modeling for the presence of adverse pathologic features, especially in settings where access to genitourinary (GU) pathological expertise may be limited.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
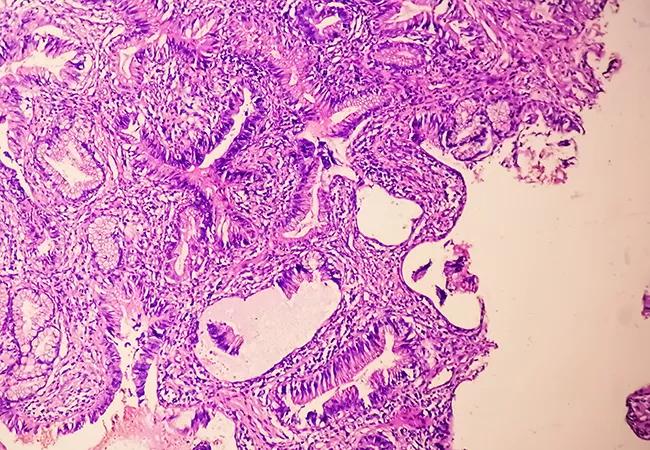
CF and IDC are morphologic features often identified in patients with Gleason grade group (GG) 3 disease. GG3 disease carries a five-fold increased risk of recurrence when compared with GG1 and GG2 disease. “Cribriform features are microscopic architectural patterns of growth in a prostate tumor that look like punched out holes, while what we call ‘intraductal carcinoma’ is another distinct pattern where we see prostatic ducts lined with basal cells and expanded by malignant epithelial cells with dense cribriform morphology or other features,” explains Christopher Weight, MD, Director of Cleveland Clinic’s Center for Urologic Oncology and coauthor of the study.
The research team retrospectively reviewed 463 patients with prostate cancer who had undergone radical prostatectomy (RP) at a single center between 2009 and 2020. Patients had a median follow-up period of 25 months. GU pathologists selected the highest-grade lesion from RP for testing and reviewed specimens for CF and IDC features, and researchers divided the patients into three groups: absent CF/IDC (CF-/IDC-), CF positive only (CF+/IDC-) and CF/IDC positive (CF+/IDC+). Genomic, pathological and clinical variables were assessed using the Pearson chi-square test. Predictors of high-risk Decipher scores were identified via multivariable logistic regression. Researchers also performed differential gene expression and gene network analysis to identify genes and gene networks associated with adverse pathologic features.
Researchers found that CF+/IDC+ patients had the highest Decipher risk scores (CF+/IDC+: 0.79 vs. CF+/IDC-: 0.71 vs. CF-/IDC-: 0.56, P < 0.001). Patients in the CF+/IDC+ group had a higher percentage of Gleason GG > 3 (CF+/IDC+: 79% vs. CF+/IDC-: 52% vs. CF-/IDC-: 52%, P < 0.001). Multivariate logistic regression demonstrated that CF+/IDC+ features on final pathology (Odds ratio [OR]: 3.94, P < 0.001) and pathologic Gleason GG > 3 (OR: 1.58, P = 0.04) were predictors of high-risk GC score.
Advertisement
“We know that invasive cribriform features and intraductal carcinoma indicate an unfavorable prognosis for patients with prostate cancer, however, these are often missed by non-GU specialized pathologists. With genomic classifiers like Decipher, community or non-subspecialized physicians may be able to identify patients at higher risk and improve patient counseling about their anticipated oncologic outcomes,” says Dr. Weight. “As a high-volume center with robust testing protocols, we fortunately have access to both expert GU pathologists and genomic testing like Decipher to allow us to reliably improve prognostic modeling for individualized risk assessment.”
These findings support recent recommendations in the field to report CF and IDC status in addition to GG and indicate that certain cases can benefit from complementary prognostic information gleaned from Decipher testing.
Researchers also performed a gene set enrichment analysis to identify any genes and gene networks associated with CF/IDC in the study group. They observed selective upregulation of developmental pathways associated with aggressive biology in prostate cancer. MYC pathway upregulation was significantly enriched in the samples from the CF+/IDC+ group of patients (normalized enrichment score [NES]: 1.65, P = 0.046). E2F targets (NES: 1.69, P = 0.031) and oxidative phosphorylation (NES: 1.68, P = 0.033) pathways were enriched as well. Upregulation of these pathways is a hallmark of luminal B subtype prostate cancer, which has worse risk scores and outcomes compared with other subtypes.
Advertisement
“These are hypothesis-generating findings, but ours is the first study to our knowledge that associates the luminal B proliferating subtype with CF/IDC features and elevated genomic risk score,” says Dr. Weight. “Our findings are a step in the direction of establishing causal molecular drivers and exploring the mechanics of cribriform and intraductal carcinoma morphology.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Approach offers a ‘middle ground’ between radical prostatectomy and active surveillance

AI histologic classifier reliably predicts clinical risk in men post-prostatectomy

Historic collaboration connects two Cleveland Clinic locations, enables real-time sharing of metrics and surgical progress
Patient factors and cancer characteristics are key to deciding between focal therapies and whole gland treatment

Novel research to evaluate noninvasive treatments in ED and chronic pelvic pain
Correlation found between the biomarker HSD3B1 and resistance to combined hormone therapy and radiotherapy

FDA-approved therapy offers promise for patients with castrate-resistant prostate cancer