Study findings call for paradigm shift in standard of care
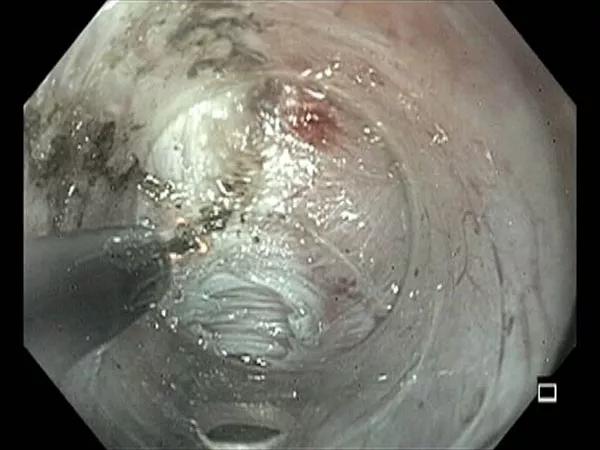
Per oral endoscopic myotomy (POEM) should be considered as first-line therapy for patients with type III achalasia. So concludes a new retrospective analysis that found the minimally invasive procedure yielded symptom relief and improved esophageal manometry, radiograph measurements and drainage studies, all with low associated morbidity.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The single-center investigation from Cleveland Clinic — one of the largest studies devoted exclusively to type III achalasia, a rare and difficult-to-treat subtype of the condition — was recently published online in the Journal of Thoracic and Cardiovascular Surgery.
“We had excellent perioperative outcomes and sustained postoperative palliation with POEM for type III achalasia at one year,” says Cleveland Clinic thoracic surgeon Monisha Sudarshan, MD, who shared first authorship of the study with Siva Raja, MD, PhD, Surgical Director of the Center for Esophageal Diseases. “Outcomes were superior to those historically reported after laparoscopic Heller myotomy, botulinum toxin injection and pneumatic dilation, suggesting a paradigm shift in initial management.”
Type III achalasia is the most severe of the three Chicago classification subtypes, defined as having premature contractions in at least 20% of swallows. It is also the rarest, with fewer than 10% of achalasia patients thus classified. Its rarity makes studies assessing optimal interventions especially difficult.
Challenges in treating this entity are compounded by the fact that spasms extend much higher than the esophagogastric junction (often to the mid-esophagus), making conventional therapies for type II achalasia, which target the lower esophageal sphincter (LES), more likely to fail.
Compared with laparoscopic Heller myotomy, POEM provides a longer proximal myotomy (7-10 cm starting in the mid-esophagus), potentially making it a better intervention for type III achalasia.
Advertisement
Using Cleveland Clinic’s prospectively maintained achalasia database, the researchers identified 504 patients treated for achalasia from April 2014 to July 2019. Of these, 217 patients (43%) underwent POEM, and 36 of those had type III achalasia, representing the study cohort.
Of the 36 patients who underwent POEM for type III achalasia (mean age, 62 years; 61% male), 11 had undergone previous interventions: botulinum toxin injections to the LES (n = 7), laparoscopic Heller myotomy (n = 3) and pneumatic dilation (n = 1).
Median operative time was 85 minutes, and median hospital stay was 1 day. Patients reported a return to activities of daily living in a median of 7 days and were followed for a median of 1 year.
The primary outcome measure was postoperative Eckardt score; 94% of patients achieved the threshold for treatment success — defined as a score ≤ 3 — at their two-week postoperative visit and through a year of follow-up.
Patients’ preoperative-to-postoperative changes in overall Eckardt score and various components of the score were as follows:
Complications occurred in three patients, as follows:
Advertisement
Esophageal pH studies were conducted about three months postoperatively in 23 patients; 14 of these (61%) had an abnormal DeMeester score (> 14.72).
Type III achalasia patients in the database who underwent laparoscopic Heller myotomy between January 2006 and July 2019 were also assessed. Thirty-five patients were identified, though the authors note that they were more similar to patients with type II achalasia since they had limited esophageal spasms.
Comparisons between the Heller myotomy and POEM cohorts were as follows:
Subsequent therapy was required by zero of 36 patients in the POEM cohort as compared with two of 35 patients in the laparoscopic Heller myotomy cohort.
The authors emphasize the following points from this study:
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years