Advertisement
Next-generation sequencing powers diagnostic tools and targeted therapies, helping drive down cancer death rates.

The overall cancer death rate in the United States has been steadily declining since the 1990s, falling by 33% between 1991 and 2021, and today more than 18 million cancer survivors are living across the country, according to the 2024 Cancer Progress Report issued in September by the American Association of Cancer Research.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Improvements in cancer prevention, detection, diagnosis, and treatment are contributing to increased survivorship, and in many areas next-generation sequencing (NGS) is a key factor. Commercially available since 2005, NGS involves the parallel sequencing of millions of small DNA fragments. It allows for the comprehensive analysis of entire genomes or large portions of them.
Today, NGS is widely used to detect mutations in cancer-related genes, helping to identify specific types of cancer and their genetic drivers.
“In the past two decades, next-generation sequencing has revolutionized cancer care and become an integral part of precision oncology,” says Kelley Kozma, DO, Cancer Center Director of the Robert and Carol Weissman Cancer Center at Cleveland Clinic Martin Health. “It’s enabling more accurate diagnoses, personalized treatments, and better outcomes for patients.”
Of all its potential applications, Dr. Kozma is most excited about the use of NGS to develop liquid biopsies that can analyze circulating tumor DNA (ctDNA) in blood for cancer detection. Already there are single-cancer and multi-cancer early detection blood tests on the market and many others in development, though they are currently most effective at identifying later stage disease.
For example, the Shield™ blood test, which was approved by the FDA this past summer for colon cancer screening, was found to have an 83% sensitivity for colorectal cancer but only a 13% sensitivity for advanced precancerous lesions, according the findings of the ECLIPSE trial.
Advertisement
“In the next five to 10 years, I expect we’ll see even more progress made in developing blood tests that can screen for early-stage disease before symptoms appear,” says Dr. Kozma. “I look forward to a future without screening mammography and when primary care providers can order a simple blood test to screen their patients for ovarian and pancreatic cancers.”
Perhaps the biggest impact NGS is currently having on cancer survivorship is through its role in treatment planning. The identification of genetic mutations specific to a patient’s cancer allows for the selection of targeted therapies that can be more effective and potentially do less harm.
At the Robert and Carol Weissman Cancer Center in Stuart, Florida, NGS is used for almost all patients who have advanced cancer, as well as patients who are elderly or who have other complications that would make it difficult for them to tolerate chemotherapy.
“We can test for over 800 different gene mutations, which potentially gives us 800 targets to go after,” says Dr. Kozma. “This opens the way for us to use targeted therapy instead of chemotherapy for certain patients.”
Patients with non-small cell lung cancer (NSCLC), the most common type of lung cancer, have benefited significantly from targeted therapies identified through NGS. For example, NSCLC tumors known to have epidermal growth factor receptor (EGFR) or anaplastic lymphoma kinase (ALK) fusion mutations can now be treated with therapies that specifically inhibit the activity of these mutated proteins.
Advertisement
“Being able to provide an oral medication instead of cytotoxic chemotherapy for certain patients with EGFR-positive disease is more efficacious and an important quality-of-life benefit,” Dr. Kozma explains. “In other cases, patients with advanced disease may undergo chemotherapy followed by targeted therapy, which can provide a better survival benefit.”
Reflecting the tremendous progress made with these more effective treatments, this year’s update to the National Comprehensive Cancer Network guidelines for NSCLC is focused on targeted therapy recommendations for patients with advanced or metastatic disease with actionable molecular biomarkers, like EGFR mutation and ALK rearrangement. Since 2022, the guidelines have recommended molecular testing in all patients with metastatic nonsquamous NSCLC and NSCLC not otherwise specified.
“Precision medicine has gone from a trend to a standard in oncology treatment,” says Dr. Kozma.
But the application of NGS goes beyond treatment selection. It can be used to assess how well a treatment is working by identifying changes in the genetic profile of tumors over time.
“This allows us to identify when the cancer develops resistance mutations,” says Dr. Kozma. “We can then switch tactics and use alternate therapies.”
NGS is also used to detect very low levels of cancer cells remaining after treatment. Signatera™ is one such test that uses ctDNA to detect minimal residual disease, which helps in the early intervention of relapsing disease.
“This test is personalized for each patient and requires both tissue and blood samples to create,” describes Dr. Kozma. “We use it for some patients with breast cancer and other solid tumors to see if the cancer has come back.”
Advertisement
She also points to the use of genetic information obtained from NGS to help predict the likely course of the disease and the patient’s response to treatment, which can help guide decision-making.
“Knowing a tumor’s characteristics has helped in so many ways,” adds Dr. Kozma. “It’s very gratifying to have access to so much actionable information that ultimately improves patient outcomes.”
Today, NGS is advancing cancer research by providing researchers with comprehensive data needed to understand cancer biology, discover new biomarkers, and develop novel therapies. It is also helping match patients with clinical trials based on their tumor’s genetic profile.
“The cost of next-generation sequencing has decreased significantly in recent years, which has fueled the growth in cancer research, especially in the area of mutation-specific targeted therapies,” says Dr. Kozma.
Cleveland Clinic has 10 clinical trials underway at the Robert and Carol Weissman Cancer Center and 55 active oncology trials at the Maroone Cancer Center in Weston, Florida. Among the studies currently enrolling patients at Cleveland Clinic Martin Health are the ASCENT-05 trial for triple-negative breast cancer and the MDT-BRIDGE trial for resectable or borderline-resectable Stage IIB–IIIB NSCLC.
“Both of these trials are assessing the efficacy and safety of treatments involving targeted therapies,” reports Dr. Kozma. In addition, the MDT-BRIDGE is investigating ctDNA as a potential biomarker by looking at associations with pathological and clinical outcomes.
Advertisement
For more information on clinical trials at Cleveland Clinic in Florida, visit Florida Cancer Research & Clinical Trials | Cleveland Clinic Florida.
Advertisement

Urologic surgeon at Cleveland Clinic Indian River Hospital performs irreversible electroporation for select cases of localized prostate cancer.
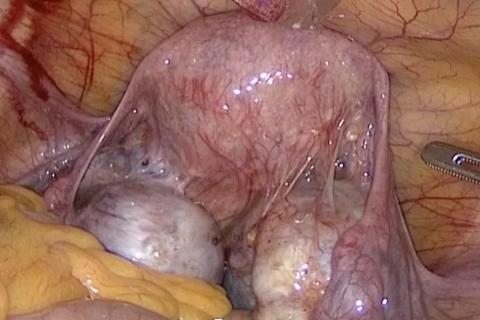
Surgeons at Cleveland Clinic Weston Hospital demonstrate the latest approaches to treating gynecological cancer