An overview of our leading-edge diagnostics and therapeutics
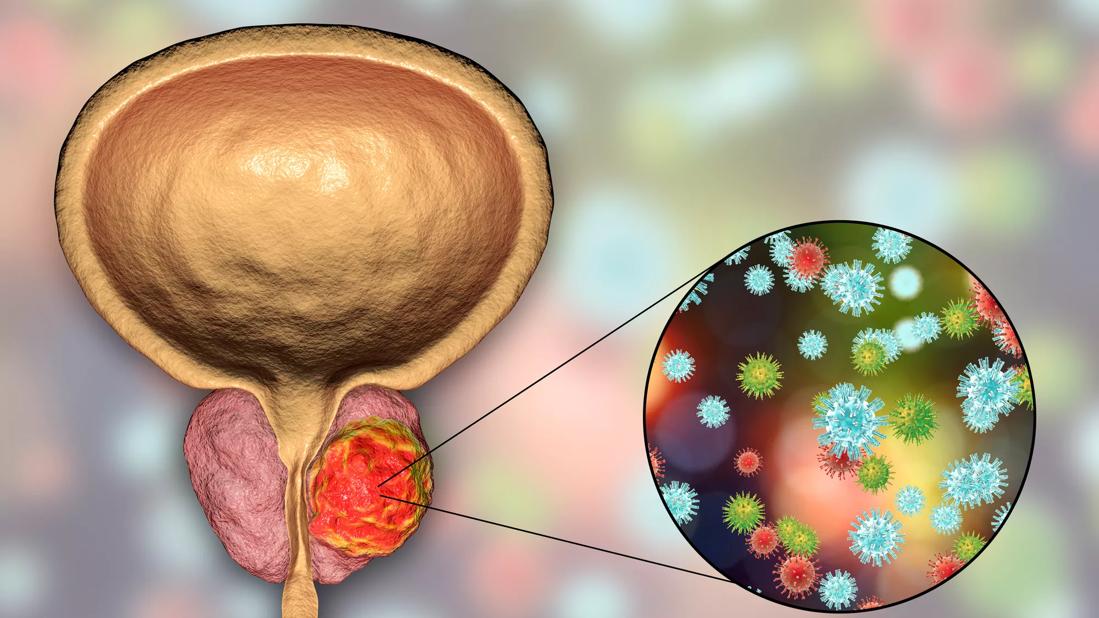
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/76eef579-9f20-4b97-aa6f-e277461a6efb/GettyImages-872569336-jpg)
Prostate cancer treatment
Experts at Cleveland Clinic have dedicated their careers to transforming the diagnosis and treatment of prostate cancer and providing individualized, high-quality care to patients. Learn more below about examples of groundbreaking research and new medical and surgical approaches that are leading the way in prostate cancer care.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Cleveland Clinic became the first medical center to offer the IsoPSA™ test to patients in July 2020. Developed in partnership with Cleveland Diagnostics, Inc., the test is a novel prostate-specific antigen assay for patients with a PSA > 4ng/ml who are facing a decision on prostate biopsy.
This blood-based diagnostic test has demonstrated superiority over conventional tests in predicting the presence of high-grade prostate cancer, potentially resulting in a significant decrease in unnecessary prostate biopsies, according to Eric Klein, MD, Chair, Glickman Urological & Kidney Institute.
“Our data show that the IsoPSA test reduces unnecessary prostate biopsies by about 45% by reliably differentiating between the risks of high-grade vs. low-grade cancer or benign biopsies,” says Dr. Klein.
Read more here.
Brachytherapy for prostate cancer is one available treatment method at Cleveland Clinic for patients with localized prostate cancer. Jay Ciezki, MD, hopes widespread adoption of the modality is on the horizon, as Cleveland Clinic’s program surpasses its 6,000th patient treated.
“This is a proven, convenient treatment method for patients with localized disease,” says Dr. Ciezki, radiation oncologist, Glickman Urological & Kidney Institute. “We’ve shown that low- and high-dose brachytherapy works as monotherapy or in combination with other treatment methods for a variety of prostate cancer types, and I think all discussions of definitively managed prostate cancer treatment should include brachytherapy.”
Advertisement
Read more here.
Localized treatment — adding brachytherapy to external beam radiotherapy — appears to improve survival outcomes for men with high-risk prostate cancer, according to a large retrospective study by Cleveland Clinic researchers published in JAMA.
The retrospective review of 1,809 patient records from 12 tertiary care centers compared the clinical outcomes of men with Gleason score 9-10 prostate cancer who had received one of three treatment modalities:
The study’s data spans 2000 through 2013, providing a birds’ eye view of the evolution of treatment modalities for this aggressive form of this disease.
Read more about study design and results here.
Robotic radical prostatectomy used to require five incisions in a patient’s abdomen. Today it requires only one, using the da Vinci® SP Surgical System. Cleveland Clinic was the first U.S. medical center to begin using the single-port robot for urology procedures in late 2018. Since then, experts at Glickman Urological & Kidney Institute have used it to perform extraperitoneal prostatectomy in over 250 patients. It’s especially beneficial in patients for whom procedures would be challenging, such as in those who are obese and those who have breathing problems.
“Performing the procedure extraperitoneally has several advantages,” says Jihad Kaouk, MD, Director, Center for Robotic and Image-Guided Surgery. “By avoiding the sac in which the bowel is contained, the surgery is compartmentalized, limited to the area just around the prostate. The gas bubble in which the robotic arms work expands the peritoneum, pushing the bowel out of the way, allowing better visibility.”
Advertisement
Read more here.
High-intensity focused ultrasound (HIFU), a type of focal therapy for treating localized prostate cancer, is emerging as an alternative to more traditional treatments, such as surgery and radiation, for select patients. The modality relies on high-frequency sound waves directed at the tumor through an ultrasound probe inserted into the rectum. The high-intensity waves cause the diseased tissue to heat up and die.
Improved HIFU technology, coupled with appropriate patient selection, is enabling us to provide this modality as an outpatient procedure. Cleveland Clinic recently acquired a Focal One® machine, making it one of approximately 14 sites nationally to offer this technology. It combines ablative and imaging techniques to target tumors in the prostate, enabling an attractive 1.5-hour, non-invasive procedure for clinically indicated patients.
Read a case study here.
Improved imaging technology and a shift in diagnostic practice are making transperineal fusion-guided biopsy a popular approach among urologists at Cleveland Clinic.
In fact, Dr. Klein this biopsy technique will become the new gold standard. “It’s more accurate and more comfortable for patients, plus there is a lower risk of infection,” he says.
In transperineal biopsy, the urologist guides the biopsy needle through perineal skin and into the prostate, as opposed to the rectal wall. Though the ultrasound is still placed in the rectum, the risk for developing an infection decreases considerably, explains Dr. Klein. It’s performed under sedation or with general anesthesia, and patients tend to report a better experience, he says. Only a handful of health systems utilize this approach to biopsy.
Advertisement
This approach is particularly well-suited for patients who have a history of infection or sepsis following transrectal biopsy or those at risk for bacteremia-induced complications. It also offers easier access to the anterior prostate, which is not well sampled with transrectal biopsy.
Learn more here.
The assay Oncotype DX® Genomic Prostate Score (GPS) provides meaningful predictability associated with distant metastases (DM) and prostate cancer-specific mortality (PCSM), according to a study published in JCO Precision Oncology. Cleveland Clinic researchers developed the assay in partnership with Exact Sciences (formerly known as Genomic Health, Inc.) over a decade ago.
GPS is a diagnostic tool that allows urologic oncologists to personalize a patient’s course of treatment based on the tumor’s biology as measured by gene expression profiling. It helps identify candidates for active surveillance versus candidates for immediate therapy. Genomic testing – in conjunction with an MRI – is a standard of care in the evaluation of prostate cancer at Cleveland Clinic.
“The validity of these tests is well-documented, but we are starting to discover their clinical implications in the context of long-term outcomes,” says Dr. Klein, “and this study shows the 20-year follow-up data to corroborate that.”
Learn more here.
Advertisement
Advertisement
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality
Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches