Options expand for patients with cancer and other conditions
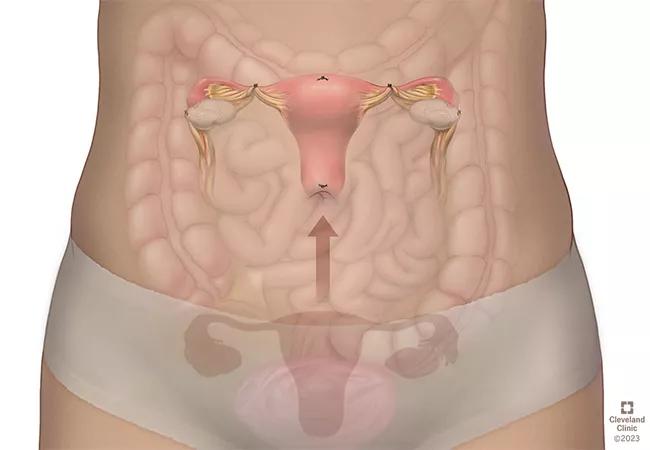
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/83bf34dd-9e73-416c-bd2d-ccb8c45f1705/Uterine-transposition-torso2-cropped-650-x-450_23-WHI-4344741_jpg)
uterine transposition
Cleveland Clinic physicians collaborating across disciplines are combining innovative interventions with well-established methods to preserve fertility for patients receiving gonadotoxic treatment for cancer.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Cleveland Clinic is really an ideal place for patients to be seen for fertility preservation, because we have so many subspecialists who can work together to individualize the patient’s treatment plan,” says Mindy Christianson, MD, MBA.
Dr. Christianson recently joined the Obstetrics & Gynecology Institute as Chief of Reproductive Endocrinology and Infertility and Practice Director of the Cleveland Clinic Fertility Center. “With oncofertility, there can be complex issues that need to be addressed. Here, the patient can see specialists in gynecological oncology, genetics and fertility, plus any other needed specialist. We can give them the most comprehensive care possible.”
Tristi Muir, MD, Chair of the Ob/Gyn Institute, says it’s important that patients and providers at peer institutions understand that Cleveland Clinic fertility care extends beyond freezing eggs.
“We really provide a lot of options, including some that are not available everywhere,” says Dr. Muir. “A person who is diagnosed with aggressive disease may need chemotherapy right away and be unable to take the time necessary for freezing eggs or embryos. If the patient doesn’t know that other options exist, and how to access them, then the future family that they have always dreamed of having could be gone.”
In addition to well-established interventions such as oocyte and embryo freezing, Cleveland Clinic’s fertility team offers ovarian tissue cryopreservation. It is the only fertility preservation option available to pre-pubertal girls and to adults who don’t have time to freeze their eggs before fertility-harming treatments begin. Often, issue harvest can be done at the time of chemotherapy port placement.
Advertisement
Cleveland Clinic also can transplant thawed cryopreserved tissue when the patient is ready to expand her family. The ovarian tissue is typically transplanted into the pelvis in the location of the ovary. The transplanted tissue starts to develop a blood supply within about 60 to 90 days, and the ovary starts to function and make estrogen and follicles. Transplanted ovarian tissue grafts typically last four to five years.
”There have been at least 300 live births to date from ovarian tissue freezing. The majority have been from transplanting the tissue back into the pelvis,” says Dr. Christianson. “There’s not a registry for these cases so the actual number of babies from frozen ovarian tissue is likely much higher. , It’s encouraging that published studies indicate that about 35% of patients achieve pregnancy after transplant.”
Ovarian tissue cryopreservation was considered experimental until 2019, and since then the fertility preservation treatment has increased in use. No live births from cryopreserved tissue have yet taken place at Cleveland Clinic, but patients have begun seeking transplantation. “We look forward to experiencing our first live birth in the near future, as patients with frozen tissue are starting to come back to attempt pregnancy,” says Dr. Christianson.
The health system also offers testicular tissue for prepubertal boys, which is still considered experimental.
For patients undergoing pelvic radiotherapy, the health system expects to soon offer uterine transposition (UT), the temporary surgical repositioning of the uterus into the upper abdomen to protect it from radiation. The procedure involves collaboration among specialists in gynecologic surgery such as gynecologic oncology and minimally invasive gynecology, radiation oncology and often colorectal surgery.
Advertisement
UT was first described in 2017. The first live birth following UT was reported in 2023 in Brazil.
“For patients with colorectal cancer, as well as patients with cervical or uterine cancer or pelvic lymphoma, treatment often requires pelvic radiation,” says Dr. Christianson. “For years, we’ve been focusing on the ovaries when it comes to fertility. Unfortunately, radiation can cause uterine fibrosis and leave the uterus less receptive to carrying a pregnancy. There are virtually no reported cases of pregnancy after pelvic radiation. For colorectal cancer, I know of no cases of a live birth after pelvic radiation because it’s so damaging.”
“We’re seeing more young women with colorectal rectal cancer, and we’re freezing their eggs and freezing embryos,” she adds. “But if we don’t move the uterus out of the radiation field, the only way they’ll be able to become a parent with those eggs or embryos is by using a gestational carrier.”
In addition to helping patients with cancer, forward-looking fertility preservation techniques also benefit patients with other conditions. For instance, patients who have receive bone marrow transplants to cure their sickle cell disease are at very high risk to develop ovarian failure.
“I have developed special protocols for patients with sickle cell disease when they freeze their eggs or freeze embryos, because they have special risks,” says Dr. Christianson. The process of stimulating the ovaries and retrieving eggs can put them at risk of sickle cell disease complications so we need to modify their treatment and collaborate closely with the hematology team.
Advertisement
Turner syndrome and certain other genetic disorders or metabolic genetic diseases elevate the risks of developing premature ovarian insufficiency, which is early depletion of the egg supply.
Fertility preservation can be done during childhood to allow patients with these conditions to become parents in the future. Still other patients may turn to fertility preservation so they can delay family building while they focus on their careers or for other reasons – this is referred to as planned fertility preservation.
For the Cleveland Clinic Fertility Center, planned fertility preservation is rapidly growing as a reason patients today are seeking consultation.
“Fertility preservation is not just about cancer,” says Dr. Christianson. “What we want physicians to understand is that whatever the fertility-related circumstances they are facing with their patients, we are here to help.”
Advertisement
Advertisement
Growing need for addressing fertility concerns
Sperm counts haven’t declined among American men in recent years, new research from Cleveland Clinic finds.
Newer drugs can affect likelihood of pregnancy
Counseling and careful surgical considerations are key
Studying trends of conization with lymph node evaluation, trachelectomy and radical hysterectomy
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine