Counseling and careful surgical considerations are key
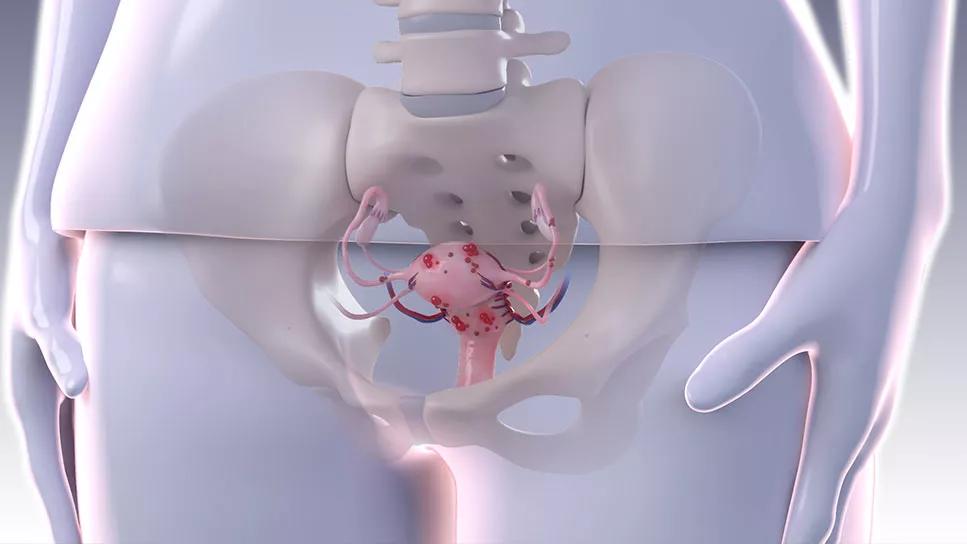
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7beffcbf-d62a-4a20-a33d-b686a703c349/fertility-preservation-with-endometriosis)
Medical illustration of endometriosis
Endometriosis, an inflammatory disease affecting an estimated 10% of reproductive-age women, is increasingly recognized by primary care providers and the public as a common cause of pelvic pain and infertility. Perhaps still underappreciated, however, is the potential effect of surgery on fertility via iatrogenic damage to the ovaries. When counseling patients with endometriosis, physicians should consider the implications of potential surgery and options for fertility preservation.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“It’s important for reproductive surgeons to evaluate the latest fertility data surrounding various surgical techniques to treat endometriosis,” says Elliott Richards, MD, PhD. “For the surgical patient desiring future fertility, a critical question should always be: How might my planned surgery impact my ability to conceive and/or respond to fertility treatment?”
In a recent article in the Journal of Clinical Medicine, Dr. Richards and colleagues in Cleveland Clinic’s Obstetrics and Gynecology Institute reviewed strategies for fertility preservation and surgical techniques to minimize iatrogenic injury to healthy ovarian tissue.
Mechanisms for endometriosis-related infertility vary and include inflammatory mediated oocyte damage and, in advanced-stage disease, distorted pelvic anatomy. However, the potential for injury during surgical treatment is another principal factor. Before deciding on treatment, consideration must be given to the level of disease and the patient’s age and reproductive goals.
“If a patient has minimal to moderate endometriosis, there is good evidence that surgical treatment of lesions will likely improve their natural fertility,” says Dr. Richards. “Conversely, for patients with advanced stage disease, undergoing surgery — especially repeat surgery — is less likely to improve fertility and can directly and adversely affect ovarian reserve, making some fertility treatments less successful.”
Many patients fall somewhere between those scenarios, which underscores the importance of thoughtful physician-patient discussion and selection of fertility preservation techniques before surgical management of endometriosis.
Advertisement
“I am pleased that fertility preservation in the context of cancer — often referred to as oncofertility — has received increased attention and funding in recent years. There absolutely needs to be similar attention given to fertility preservation in the context of advanced-stage endometriosis,” says Dr. Richards.
The mainstay of fertility preservation is oocyte retrieval and either egg freezing or in vitro fertilization with embryo cryopreservation. Ovarian tissue cryopreservation may be a desirable option in some scenarios, such as for patients for whom in vitro fertilization is not an option and/or who require an oophorectomy. While it may be used for control of pain symptoms, medical treatment for endometriosis does not improve fertility outcomes.
When counseling patients on fertility preservation options, key variables to consider are their desire for fertility, timeline for family building, age and ovarian reserve.
“When managing endometriomas surgically, you want to minimize harm to the ovarian cortex, where the eggs reside,” says Dr. Richards. “The surgical technique absolutely makes a difference, and techniques that minimize the use of energy devices are most beneficial.”
Cystectomy is the standard surgical approach for endometriomas, resulting in improved pain resolution, reduced recurrence, and improved spontaneous conception compared to ablative approaches. However, as it can cause greater injury to the ovarian reserve than ablative approaches, it should be used with caution in women with diminished ovarian reserve at baseline. If an ablative approach is chosen, plasma energy and laser ablation result in less injury to the ovary than electrosurgical energy.
Advertisement
As endometriosis is progressively being diagnosed earlier, it is important for gynecologists and reproductive surgeons to be knowledgeable about fertility preservation options for these patients.
“Patients are being diagnosed and treated for endometriosis at younger and younger ages, often before fertility is on their radar, while at the same time childbearing is being delayed until older ages,” says Dr. Richards. “I encourage my colleagues to bring up fertility preservation at the endometriosis surgery consult. Even if the patient elects not to proceed with preservation, having this discussion helps prevent a patient from feeling blindsided later, when they find out their ovarian reserve is extremely low, or feeling betrayed that they missed a potential window of opportunity to preserve their fertility.”
Advertisement
Advertisement
A multidisciplinary approach facilitates timely diagnosis and better treatment
Cara King, DO, MS, outlines practices that can make all the difference
Better screening can improve GI outcomes and reduce costs
A large nodule had strangulated the patient’s ureter and invaded the vagina, bladder and rectum
Case study: Concomitant robot-assisted surgery without repositioning the patient
Growing need for addressing fertility concerns
Sperm counts haven’t declined among American men in recent years, new research from Cleveland Clinic finds.
Newer drugs can affect likelihood of pregnancy