Sensitivity, specificity higher than current test
Physicians are increasingly diagnosing pancreatic cystic lesions due to expanded access and use of cross-sectional imaging. Most pancreatic cysts are benign, however, it is challenging to differentiate between benign nonmucinous cysts and potentially malignant mucinous cysts. What’s more important is early and accurate diagnosis is key for curative treatment and surveillance.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The gold standard for diagnosing a precancerous cyst is surgical pathology, however, physicians would prefer a less invasive, but still accurate test to make the distinction. With that in mind, Cleveland Clinic researchers recently conducted a retrospective study to determine if measuring intracystic glucose levels within the cyst’s fluid might be more accurate than the most prevalent current test of measuring of carcinoembryonic antigen (CEA) levels within the cyst fluid.
“The sensitivity, specificity and accuracy of CEA is not that great,” says advanced endoscopist Prabhleen Chahal, MD, who presented their findings Saturday at DDW 2018. “That’s what led us to study this very simple, easy, quick and cost-effective method of measuring intracystic glucose levels.”
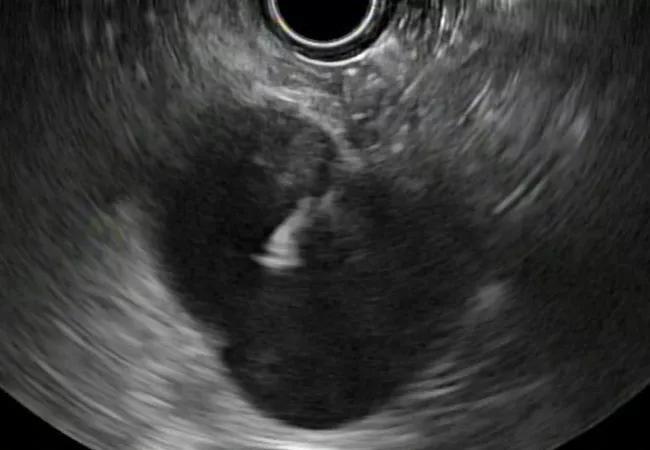
The study cohort consisted of 74 (23 nonmucinous and 51 mucinous) patients who had undergone endoscopic ultrasound and fine needle aspiration, FNA, between 2014 and 2017 to determine the type of cyst in their pancreas.
The mean age of the patients was 66.5 years and 46 (62 percent) were female. Mean body mass index, BMI, was 29.7. Almost half of the patients (33) had never smoked tobacco cigarettes (45 percent), whereas 26 patients were former smokers (35 percent) and 15 were current smokers (20 percent).
Twenty-two were alcohol users (30 percent), 23 had a history of acute pancreatitis (32 percent). Finally, 30 of the cysts were located at the pancreatic head, 19 at the body, 18 at the tail, 3 at the neck and 2 were in the uncinate process.
Advertisement
Dr. Chahal and her colleagues found that the intracystic glucose levels in the patients’ cysts ranged from <2 to 144 mg/dL with a mean of 33.7 ± 43.1 and a median of 2.5 mg/dL.
Their analysis showed that intracystic glucose ≤41 mg/dl had a sensitivity of 88 percent and a specificity of 87 percent in differentiating mucinous from nonmucinous cysts. They also found that intracystic glucose with a cutoff of ≤21 mg/dl, had a sensitivity of 84 percent, specificity of 91 percent.
By contrast, they found the widely used CEA ≥ 184 ng/mL had a sensitivity of 50 percent and a specificity of 87 percent.
“Intracystic glucose was far superior than CEA,” Dr. Chahal says. “The sensitivity and specificity were better than CEA in separating precancerous mucinous from benign nonmucinous.”
In addition, she says, “CEA usually takes a few days to get back and glucose has a much more rapid turn around of less than 30 minutes. It’s also much more cost effective, simple to do and readily available. Even small community hospitals that do endoscopic ultrasound can do it within their laboratory.”
More data showing surgical corroboration of the predictive value of intracystic glucose test are needed, she says, but the results point to the measurement of cystic glucose levels as a potential game-changer for diagnosing precancerous mucinous cysts.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years