Findings could help promote organ preservation

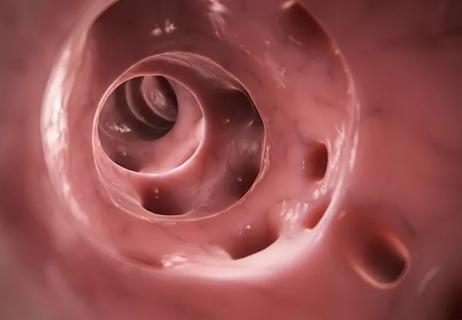
Findings from a new study demonstrated that selective use of total neoadjuvant treatment (TNT) among patients with Stage I rectal cancer has the potential to promote organ preservation, particularly for tumors located in the lower rectum.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Led by Emre Gorgun, MD, MBA, Vice Chair, Colorectal Surgery, Cleveland Clinic, this research, “Is There a Role for Total Neoadjuvant Treatment in Early-Stage Rectal Cancer,” was presented during the Digestive Disease Week Conference, held May 18-21, 2024, in Washington, D.C.
Total neoadjuvant treatment, an increasingly used approach for the treatment of locally advanced rectal cancer, offers higher complete response rates and better treatment adherence. “For early-stage rectal cancer (ESRC), total mesorectal excision is typically recommended as the initial treatment. However, impaired functions and permanent colostomy remain undesirable outcomes, particularly in low-located ESRC,” notes Dr. Gorgun. “The selective use of total neoadjuvant treatment for patients with early-stage disease may be a viable option; however, further investigation is required.”
To better understand the potential of this approach, Dr. Gorgun and colleagues initiated the current study, hypothesizing that total neoadjuvant treatment may result in organ preservation among patients with early-stage rectal cancer.
Researchers retrospectively reviewed data from early-stage rectal cancer patients who were recommended total neoadjuvant treatment between 2015 and 2023. Their analysis included patients who underwent total neoadjuvant treatment based on their choice after either initial diagnosis or transanal excision.
Fifteen patients—10 males and five females—diagnosed with T2N0 low rectal adenocarcinoma were enrolled in the study. The median age was 60 years (55.5-68.5), median tumor size measured 3.1 cm (2.5-3.9), and the median distance from the top of the internal anal sphincter (IAS) was 0.2 cm (0-1.4), with partial sphincter (control muscle) involvement observed in six patients.
Advertisement
Of the nine patients who received total neoadjuvant treatment after initial diagnosis, seven subsequently achieved a clinical complete response. “One patient underwent endoscopic submucosal dissection (ESD) due to a near-complete response, revealing tubulovillous adenoma upon histopathological examination,” reported Dr. Gorgun and colleagues. “Another patient underwent low anterior resection and achieved pathologic complete response (pCR). Three patients underwent total neoadjuvant treatment after transanal excision.”
The overall complete response (CR) rate was 100%, according to Dr. Gg. The median follow-up period for the entire study population was 21 months. During this time period, the researchers observed no disease recurrence or mortality in either group.
“Of note, one patient who underwent total neoadjuvant treatment following their initial diagnosis was scheduled for surgery due to a rectovaginal fistula,” the study authors explain. “The remaining two patients who were recommended total neoadjuvant treatment after the initial diagnosis and one patient who received this treatment recommendation after local excision are currently continuing total neoadjuvant treatment.”
Summarizing their key findings, Dr. Gorgun reiterates, “Our data showed a complete response rate of 100% in this study population, a dramatic increase compared to the typical 40-45% response rate of locally advanced tumors when given total neoadjuvant treatment,” he reiterates. “And so, this research suggests that early-stage patients are really responsive to this approach as well and can have almost 100% organ preservation with this method.”
Advertisement
Overall, this study highlights the potential of selective total neoadjuvant treatment for patients with early-stage rectal cancer, according to Dr. Gorgun, who also notes that intersphincteric resection may have a potential advantage over abdominoperineal resection for patients who attain tumor downsizing after undergoing this treatment regimen.
In terms of next steps, Dr. Gorgun says it would be interesting to look at reducing the chemoradiation dosage. “While further studies are required, a reduced dose treatment may be effective in this group of patients, offering less side effect while still maintaining the strong response rate.”
Today, patients with early-stage rectal cancer are often treated surgically; however, this research offers a different perspective with a complete paradigm shift, notes Dr. Gorgun. “When managing these — and other — patient populations, we should not be dogmatic in the treatment options that we offer to our patients and have an open mind to newer, cutting-edge approaches in the management of complex problems. This will be beneficial for not just our patients, but the healthcare system as a whole.”
Advertisement
Advertisement

Poor response may be due to different tumor biology

Study sheds light on distant metastasis rates between upfront surgery and Watch & Wait strategies

Tips on how to recognize the condition and budesonide treatment guidance
Input from specialists and other healthcare providers is important when discussing quality-of-life improvement options

The retrospective study also identified predictors for which patients would likely achieve a complete response from TNT

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence