Multidisciplinary approach results in faster, safer access to the foramen ovale
When patients have treatment-refractory trigeminal neuralgia, percutaneous balloon compression (BC) often is a last resort for relief from debilitating facial pain. The fluoroscopically guided cannulation of the foramen ovale required, however, can be technically challenging for surgeons and fraught with risk of complications.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Neurosurgeons and interventional neuroradiologists at Cleveland Clinic Florida believe that combining BC with intraoperative intravenous contrast-enhanced DynaCT imaging is an easier, safer alternative. Their technique and positive results with the approach in 20 patients are described in a new case series published online in Neurosurgical Review.
“With DynaCT, we can precisely determine the needle path, avoiding injury to large and small vascular structures,” says case series co-author Hamid Borghei-Razavi, MD, Director of Cleveland Clinic Florida’s Minimally Invasive Cranial and Pituitary Surgery Program. “Needle insertion requires only one pass (see Figure), and the outcome for patients is much better than with pure fluoroscopically guided cannulation.”
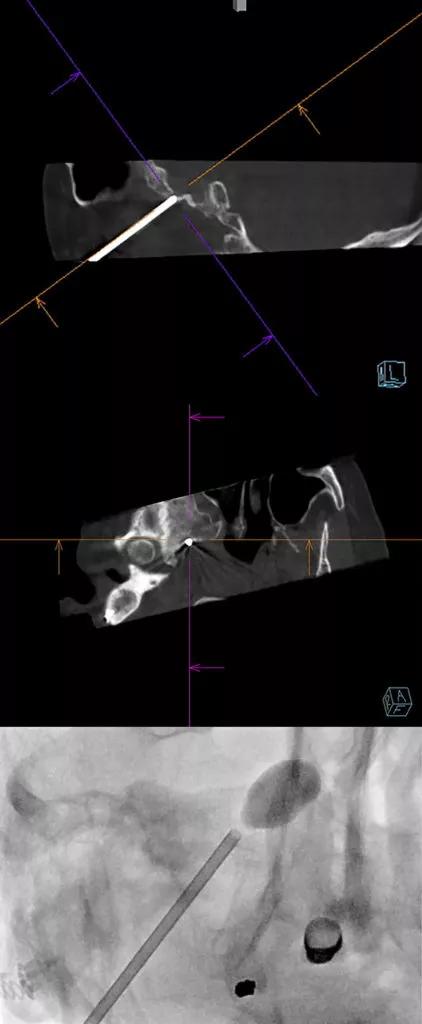
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3ac67be9-ffcc-400d-bc69-0735a6132390/21-NEU-2527834-CQD-Insets-800x1940-1-422x1024_jpg)
Figure. Top two panels demonstrate the use of intraoperative DynaCT to navigate a needle in real time in a single pass directly into the right foramen ovale. Bottom panel demonstrates the position of the inflated balloon in the right foramen ovale.
The novel approach described in the case series is an outgrowth of a multidisciplinary collaboration among experts at Cleveland Clinic. Neurosurgeons had been using X-rays as part of their preoperative planning for trigeminal neuralgia procedures, but they saw the potential for improved outcomes after hearing about DynaCT from their colleagues in interventional radiology, who were experts with it.
“This is a good example of how clinicians in different specialties can learn from each other,” says Dr. Borghei-Razavi. “Our patients with trigeminal neuralgia are more satisfied and have less pain and soreness after the procedure.”
Advertisement
“In most medical systems, physicians are organized by treatment modality, with little direct interaction between medical, surgical and radiological specialties,” adds Michal Obrzut, MD, Director of Neurointerventional Radiology at Cleveland Clinic Florida and a co-author of the case series. “Surgeons operate in the OR, while radiologists read films in their cubicles. At Cleveland Clinic, however, our multidisciplinary institutes unite all specialists in a given area under one umbrella. Our Neurological Institute includes the Pauline Braathen Neurological Center, where neurosurgeons, neurointerventionalists and neurologists all sit together. This enhances opportunities for collaboration and cutting-edge research — and ultimately results in better patient outcomes.”
All 20 patients in the case series had previously been treated for trigeminal neuralgia with medication or other interventions. Eight had undergone microvascular decompression, four had undergone rhizotomy and two had undergone stereotactic radiosurgery. Patients’ average age was 65 years, and 18 had comorbidities, including heart disease, hypertension, hyperlipidemia, diabetes mellitus or cancer.
Pain from trigeminal neuralgia was assessed using the Barrow Neurological Institute (BNI) pain intensity score. Patients’ preoperative pain scores were as follows:
As of publication of the case series and based on six- to 12-month follow-up, none of the patients treated with percutaneous BC using intraoperative contrast-enhanced DynaCT had experienced a relapse of their presenting pain symptoms. Immediately after the procedure, 10 patients had complete relief from pain (BNI score I), six had a > 50% improvement and four had minimal initial improvement. Of the latter four patients, two continued to experience atypical trigeminal neuralgia over follow-up.
Advertisement
None of the patients had complications. In contrast, the authors note, the traditional technique for plotting the needle trajectory can be associated with inadvertent injury to blood vessels in individuals with tortuous carotid arteries or variant anatomy.
Unlike the technique described in previous reports of DynaCT use in this setting, the one used by the Cleveland Clinic researchers does not depend on a predetermined entry point or Härtel’s landmarks.
According to the authors, the average radiation dose area product and total fluoroscopy time for their procedures were 3,267.48 µGym2 and 45 seconds, respectively. In comparison, the average radiation dose for percutaneous BC without DynaCT is approximately 1,137.18 µGym2 with an average fluoroscopy time of 62 seconds.
“Some may note that this technique increases the dosage of radiation,” Dr. Borghei-Razavi acknowledges, “but using DynaCT eliminates the need to perform a CT scan before surgery to visualize the foramen ovale, which avoids a different source of radiation exposure for patients.”
Aside from pre-planning the 3D path of the needle, the neurosurgeons also use DynaCT to confirm the final position of the needle before insertion and after inflation. They believe their use of this technology in collaboration with their interventional radiology colleagues allows them to more selectively target trigeminal nerve branches.
Since this published case series, Cleveland Clinic Florida neurosurgeons and interventional neuroradiologists have used percutaneous BC and intraoperative contrast-enhanced DynaCT to treat an additional 15 patients with trigeminal neuralgia, with similar results. The next step is long-term evaluation of the original cohort — and possibly another advance in technology.
Advertisement
“We currently use a Fogarty balloon for these procedures, but we are developing a balloon specifically for surgery on the foramen ovale,” says Dr. Borghei-Razavi. “We hope this will result in even greater accuracy and outcomes in the treatment of refractory trigeminal neuralgia.”
Advertisement
Advertisement
Nonthermal technique reduces bleeding and perforation risk
Standardizing a minimally invasive approach for Barrett’s Esophagus and Esophageal Cancer
PSMA-targeted therapy for metastatic prostate cancer now offered at Cleveland Clinic Weston Hospital
Nationally recognized urologic oncologist offers vision for growth, innovation, and excellence
Noninvasive modality gains ground in United States for patients with early-to-moderate disease
Cleveland Clinic Weston Hospital’s collaborative model elevates care for complex lung diseases
Interventional pulmonologists at Cleveland Clinic Indian River Hospital use robotic technology to reach small peripheral lung nodules
Trained in the use of multiple focal therapies for prostate cancer, Dr. Jamil Syed recommends HIFU for certain patients with intermediate-risk prostate cancer, especially individuals with small, well-defined tumors localized to the lateral and posterior regions of the gland.