Multi-institutional registry analysis highlights need for further research
An analysis of the largest recorded cohort of patients with invasive lobular breast cancer (ILC) demonstrates that outcomes are significantly worse when compared with invasive ductal breast cancer (IDC), highlighting a significant need for more research and clinical trials on patients with ILC. This clinical and pathological, multi-institutional, epidemiological cohort study provides prognostic insights critical to future research and clinical trials and was presented at the 2020 San Antonio Breast Cancer Symposium.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Many of us in the community feel like these cancers need some special attention,” says Megan Kruse, MD, a hematologist/oncologist at Cleveland Clinic Cancer Center and senior author of the study. “That maybe it’s not best that we treat lobular breast cancer the same as ductal breast cancer. But the challenge in doing so is that lobular breast cancer cases are pretty rare, and so in order to really get a comprehensive look at its characteristics and treatment patterns, you really have to do it across multiple institutions.”
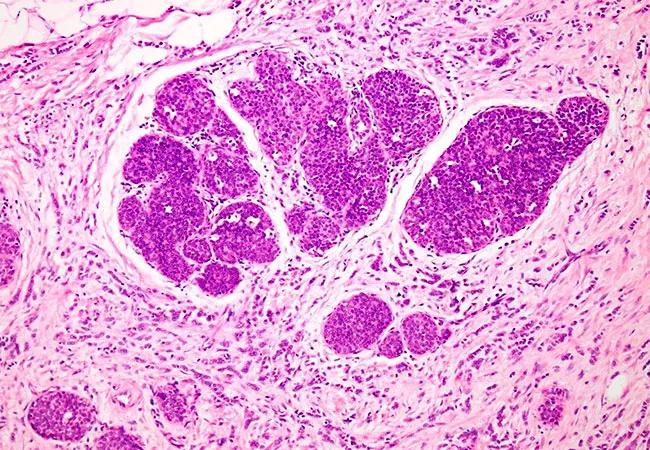
Lobular breast cancer is the second most common type of breast cancer from a histological perspective, but it only represents about 10 to 15 percent of breast cancer cases. Because of its rareness, oncologists have tended to view it and treat it in the same way as the more common ductal breast cancer.
But as more research is performed on lobular cancers, investigators are starting to recognize that it has some distinct features apart from ductal cancer, especially with respect to how it metastasizes and its decreased sensitivity to chemotherapy.
With this in mind, scientists from Cleveland Clinic, University of Pittsburgh Medical Center and Ohio State University have created a lobular breast cancer registry that will include cases from 1990 to the present. The present study is one of the first from this newly created registry.
The pooled registry included 38,175 records, 30,1000 of which were IDC (89.3%) and 3,618 of which were ILC (10.7%). Researchers did not find significant differences between the cancer groups in either laterality or body mass index. However, the data revealed that ILC patients were significantly older (61.2 vs. 57.5 years; P < 0.0001), and that African American patients made up a greater percentage of IDC patients (7.6% vs. 9.2% in ILC vs. IDC, respectively; P = 0.004).
Advertisement
Patients with lobular breast cancer had fewer grade III tumors (11.4% vs. 40.3% in IDC; P < 0.0001) and significantly larger tumors than IDC (13.7% T3 vs. 2.8%, P < 0.0001). Patients with ILC were more frequently in stage III (16.6% vs. 8.0% in IDC) and stage IV (3.7% vs. 2.4% in IDC) (P < 0.0001). ILC patients also had more lymph node involvement (P < 0.0001).
The cohort of patients with ILC also had lower rates of HER2+ cases (5% vs. 18.1% in IDC; P < 0.0001) and a lower proportion of patients with high Oncotype Dx Recurrence Scores (P < 0.0001). More patients with ILC had estrogen receptor (ER)-positive tumors (P < 0.0001).
Logistic regression analysis was performed, and age, stage, grade, lymph node involvement, HER2 and ER status remained significantly associated with histology. Kaplan-Meier analysis revealed that patients with ER+ ILC have significantly shortened disease-free survival (DFS) (P = 0.041) and overall survival (P < 0.0001). Estimated DFS rates confirmed prior data showing late recurrences in patients with ILC.
“The most important finding from this analysis is the mounting evidence that we need to pay attention to late recurrences for ILC patients. The registry also includes important data on patterns of recurrence, and we intend to dive deeper into metastatic patterns and survival outcomes,” says Dr. Kruse.
This study is the first of many planned which are enabled by the volume of patients and close collaboration among the institutions of the Great Lakes Breast Cancer Consortium.
Advertisement
“Our next steps are to look at the type of treatments patients received: who got chemotherapy, who didn’t and how they responded,” says Dr. Kruse. “We would also love to be able to look at the types of endocrine treatment received along with the duration of treatment. This is a very relevant clinical question that is unlikely to be able to be answered in a prospective trial.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors