Large data analysis finds cancer helps predict stroke risk in patients with atrial fibrillation
Breast, colon, lung and prostate cancers should be considered for inclusion in the CHA2DS2VASc model for stroke prediction in patients with atrial fibrillation (AF), concludes a database analysis of more than 100,000 patients published by Cleveland Clinic investigators in the International Journal of Cardiology: Heart and Vasculature (2022 Jun;41:101072). The study found that the presence of one of these cancers increased the risk of stroke in AF patients to a degree comparable to that of age over 75 years, female sex and diabetes — all variables in the current model.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Cancer increases risk across the whole spectrum of CHA2DS2VASc scores,” says the study’s corresponding author, Rohit Moudgil, MD, PhD, a cardiologist in Cleveland Clinic’s Section of Clinical Cardiology. “Adding cancer to the tool will allow offering anticoagulation therapy to more patients in need of it.”
The CHA2DS2VASc tool for predicting stroke risk in AF takes into account congestive heart failure, hypertension, age, diabetes, history of stroke, vascular disease and sex. The score is widely used to determine whether a patient with AF should be on prophylactic anticoagulation therapy.
Prior evidence indicates that cancer increases the risk of developing AF, likely owing to the disease itself and associated therapies. In addition, an association between cancer and risk of venous thromboembolism and stroke has been demonstrated.
Despite significant evidence linking cancer and thromboembolic stroke, whether cancer is an independent risk factor for stroke in patients with AF has not been adequately studied.
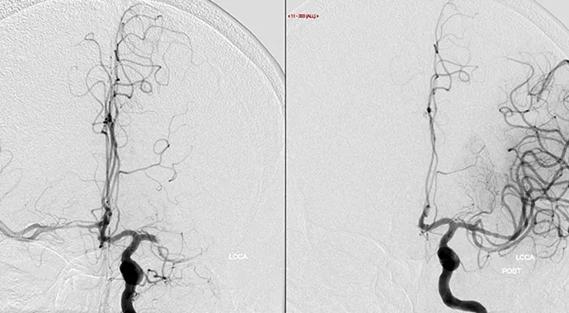
The investigators searched the national Surveillance, Epidemiology, and End Results (SEER) registry for cancer surveillance from 2007 through 2016 to identify cases of new incident AF among patients with the four most commonly diagnosed cancers in the U.S.: lung, colon, breast and prostate cancer. Patients with a history of stroke or transient ischemic attack before the diagnosis of AF were excluded. The resulting 48,242 patients with cancer and newly diagnosed AF were compared with a control group of 52,943 non-cancer patients with newly diagnosed AF from the same dataset.
Advertisement
The primary endpoint was incidence of stroke per 100 person-years. For each patient, the CHA2DS2VASc score was calculated (maximum score was 7, given that patients with prior stroke were excluded) and compared with a model that included cancer in the score. A propensity-matched cohort analysis with groups having equivalent CHA2DS2VASc scores was also conducted to compare stroke-free survival. All patients were matched, yielding 48,242 pairs.
Major findings included the following:
The researchers note that this study’s findings are bolstered by its inclusion of 10 years of data, which represents much longer follow-up than in any previous studies of this type.
Advertisement
They add that greatest impact of the proposed new CCHA2DS2VASc score is that cancer’s predictive power was comparable to age greater than 75 years, female sex and diabetes. “The strength of the CHA2DS2VASc model over the previously used CHADS2 was its ability to identify those who are and are not truly at risk,” they write. “[T]he addition of cancer as a variable in this model will further improve on this.”
The authors also note that adding cancer as a variable will enable more patients at risk to start anticoagulation therapy. Among the cancer cohort, 3.1% had a traditional CHA2DS2VASc score of less than or equal to 1 — a group that would be deemed low risk under the traditional model and not eligible for anticoagulation therapy.
“This study offers compelling evidence to add the presence of lung, colon, breast or prostate cancer to the current CHA2DS2VASc tool,” says Dr. Moudgil. “However, more research is warranted before adopting this plan.” He notes that the investigators hope to pursue future research to assess the effect of cancer stage on stroke risk and the effect of additional types of cancer (e.g., pancreatic) beyond the four common malignancies included in this study.
“While there are limitations inherent to the study’s observational nature and possibly residual confounding due to the inability to identify patients on anticoagulation therapy, the findings are interesting,” says Ayman Hussein, MD, of Cleveland Clinic’s Section of Cardiac Electrophysiology and Pacing, who wasn’t involved in the study. “While cancer increases the risk of thrombosis, further research and analysis is needed to substantiate the addition of cancer to stroke risk assessment in AF patients,” adds Oussama Wazni, MD, MBA, Section Head of Cardiac Electrophysiology and Pacing.
Advertisement
Dr. Moudgil concurs. “We must be mindful that the risk of bleeding in cancer patients is also elevated, especially in patients receiving anticoagulation,” he says. “Therefore, the risk-to-benefit ratio needs to be calculated on an individual basis to see if the patient will benefit from anticoagulation — a calculation which is done in clinical situations on a daily basis.” Dr. Moudgil is currently engaged in active research where anticoagulation and the resultant bleeding will be factored into the scoring system. “This publication is a stepping stone to future research which will bring about a change in how we manage our cancer patients who have atrial fibrillation,” he concludes.
Advertisement
Advertisement

Aim is for use with clinician oversight to make screening safer and more efficient

Increasing treatment options are extending the window for continued functional gains
Study links large artery atherosclerosis and delayed presentation to poorer treatment results

$3.2 million grant will fund use of calcium-based imaging to record neuronal activity in ischemia model

Findings from large cohort analysis can guide ongoing quality improvement initiatives

Insights and what’s next for the first U.S. mobile stroke unit to treat patients

Research to test clinical efficacy and cost-effectiveness versus standard-of-care rehab

Times to target blood pressure, CT and medication administration shorter than with EMS transport