Study links large artery atherosclerosis and delayed presentation to poorer treatment results
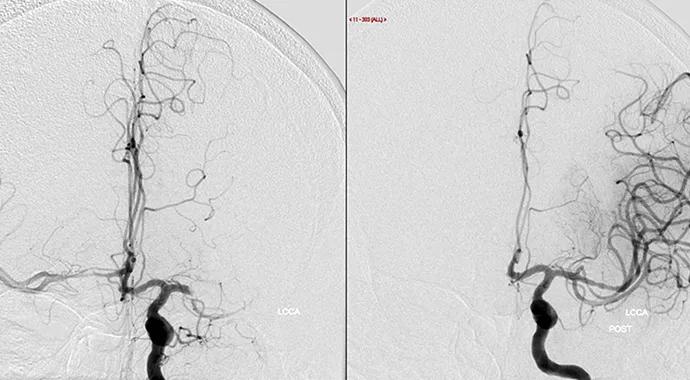
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0989e6c2-e983-4c90-a53f-e5c551c86f7b/MrClean-690x380_jpg)
large vessel occlusion before and after treatment
Outcomes are good for adults aged 18 to 49 years with large vessel occlusion acute ischemic stroke (LVO-AIS), irrespective of etiology. The exception is large artery atherosclerosis (LAA), which is associated with worse stroke scores on discharge.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
These findings from a retrospective Cleveland Clinic cohort study — one of the largest studies of young adults with LVO-AIS focused on the effect of stroke etiology on treatment-related outcomes — were published in the Journal of Stroke and Cerebrovascular Diseases (2024;33[12]:108027).
“To my knowledge, this is the first study of LVO-AIS from Cleveland Clinic and one of the first to focus exclusively on young adults,” says corresponding author G. Abbas Kharal, MD, MPH, a stroke neurologist and immunologist in Cleveland Clinic’s Cerebrovascular Center. “It shows that LVO-AIS is not uncommon in this population, and while the etiology is mostly cryptogenic, treatment with thrombolysis plus thrombectomy leads to good outcomes.”
LVO-AIS is historically thought to be less common in adults younger than 50 than in older individuals, but such cases have increased over the past two decades as the global incidence of stroke in younger populations has continued to grow.
While stroke mechanisms are known to differ between young and older adults, literature about younger patients with LVO-AIS is limited. The available data suggest that cardioembolism and dissection may be common etiologies of LVO-AIS in this population and that the underlying cause remains undetermined in nearly one-third of cases.
Acute treatments for patients with salvageable brain tissue include intravenous thrombolysis (IVT) if presentation is within 4.5 hours of last known well time (LKW) and mechanical thrombectomy (MT) if presentation is within 24 hours.
Advertisement
A meta-analysis of six randomized controlled trials of mechanical thrombectomy in adults showed that young adults (ages 18-49) did not benefit from MT as much as older adults did. “There is limited data focusing on young adults with LVO-AIS,” Dr. Kharal notes, “so we sought to better understand why LVO-AIS occurs in younger adults and whether treatment affects their clinical outcomes — a question that is crucial to improve care for these patients.”
Data for the new research were from 1,210 patients aged 18 to 50 treated for AIS between January 2017 and December 2021 at any of Cleveland Clinic’s 10 primary or comprehensive stroke centers in Ohio. Of these patients, 220 had LVO on computed tomographic angiography/magnetic resonance angiography.
The researchers divided the patients with LVO-AIS into five groups based on treatment received: IVT only, MT only, IVT+MT, no treatment and unsuccessful MT. Demographics, stroke etiology as defined in the TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification and treatment outcomes were assessed.
The goal was to determine the effect of stroke etiology and treatment on clinical outcomes in young adults with LVO-AIS. NIH Stroke Scale (NIHSS) score at discharge and 90 days and interactions between treatment and stroke etiology were analyzed with multivariable linear regression models.
Median age was 42 years (interquartile range [IQR], 36-46). Stroke etiology, per TOAST, was undetermined in 34.7% of patients, cardioembolism in 19.2%, large artery atherosclerosis in 17.4% and “other determined etiology” in 28.6%, which was consistent with previous studies.
Advertisement
Eighty-four patients underwent MT, in whom it was successful in 75 and unsuccessful in 9. Twenty-six patients received IVT. Neither intervention was received by 110 patients.
Thrombectomy outcomes were favorable (TICI 2b/2c/3) in 87.2% of patients who underwent it. “This compares well with the 64.2% favorable rate in the MR CLEAN registry substudy, which compared treatment in younger and older adults,” Dr. Kharal notes. “It also shows that younger adults have outcomes with thrombectomy that are as good as, if not better than, those in older adults.”
Median lag time from LKW to presentation was longest for patients who received neither MT nor IVT. Of those patients, 35% with an initial NIHSS score ≤ 5 and 25% with an initial score ≥ 6 presented more than 24 hours after LKW.
NIHSS score at discharge averaged 3 points lower in patients who had IVT+MT than in those who received neither treatment (P = .038). It was also lower in patients with IVT+MT in all TOAST categories except large artery atherosclerosis.
“Fifty percent of patients with LVO-AIS in our study received no acute intervention, and for approximately 25% of them, it was because they arrived too late,” Dr. Kharal observes. “Had they arrived earlier, they could have been eligible for IVT and possibly both IVT and MT.
“Raising awareness about stroke in young adults is paramount,” he continues, “because patients who presented the earliest and received IVT+MT had more favorable outcomes. We need to understand the barriers to delayed presentation in this population and find ways to overcome them. Our findings also underscore the importance of raising awareness among young adults about the signs of stroke, the need to seek immediate medical treatment for acute stroke symptoms and the importance of addressing stroke risk factors to reduce risk in young adults.”
Advertisement
Advertisement
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Aim is for use with clinician oversight to make screening safer and more efficient
Increasing treatment options are extending the window for continued functional gains
$3.2 million grant will fund use of calcium-based imaging to record neuronal activity in ischemia model
Findings from large cohort analysis can guide ongoing quality improvement initiatives
Insights and what’s next for the first U.S. mobile stroke unit to treat patients
Research to test clinical efficacy and cost-effectiveness versus standard-of-care rehab
Times to target blood pressure, CT and medication administration shorter than with EMS transport