The relationship between MTHFR variants and thrombosis risk is a complex issue, but current evidence points to no association between the most common variants and an elevated risk

By Andrew Dhawan, MD, DPhil and Charis Eng, MD, PhD
Polymorphisms of the methylene tetrahydrofolate reductase (MTHFR) gene are common among the general population, and data from large meta-analyses do not support the association of these variants with elevated prothrombotic risk. Clinicians should educate patients with MTHFR polymorphisms about the lack of evidence for association with thrombotic risk and focus on addressing modifiable thrombotic risk factors.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
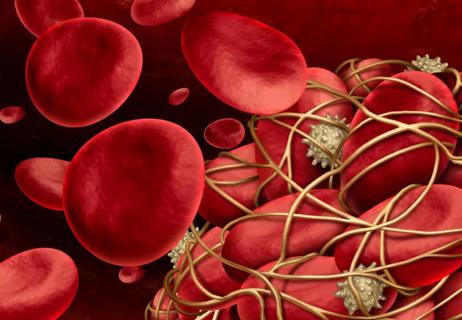
MTHFR is an essential enzyme that is encoded by the MTHFR gene, which catalyzes the conversion of 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, the primary form of folate in circulation. This substance, 5-methyltetrahydrofolate, is also a necessary cofactor for the conversion of homocysteine to methionine, required for protein synthesis.1 Reduced expression of MTHFR has been implicated in elevated serum homocysteine and reduced serum folate levels, a condition known as hyperhomocysteinemia.2–4 The relationship between serum homocysteine levels and disease has been investigated across several disease states. In this review, we focus on its putative relationship with venous thromboembolism (VTE).
Single nucleotide polymorphisms (SNPs) and single nucleotide variants (SNVs) both refer to single base-pair changes in the nucleic acid sequence of a gene, but they are not interchangeable terms. SNVs are changes that occur in less than 1% of the population, whereas SNPs occur in at least 1% of the population.5 Neither of these terms implies pathogenicity of the genetic change, and both may be colloquially referred to as “mutations.” It should also be noted that databases cataloging human genetic variation are biased toward populations with Northern European heritage. There are fewer patients with African, South American, Indigenous, Pacific Islander, and Southeast Asian heritage in the databases, complicating the estimation of true population prevalence for a given genetic variant.
Advertisement
From an epidemiologic perspective—because SNPs in MTHFR are common, some occurring in up to 40% of the general population—achieving statistical significance for an association between SNPs and a clinical variable of interest is subject to many potential biases.6 It is important for the clinician to recognize potential sources of confounding in these studies.
First, not all MTHFR SNPs are equivalent, and different SNPs should be considered independently as risk factors, as should homozygosity and heterozygosity. Second, correlation does not imply causation, and epidemiologic studies can provide correlative evidence, but confounding effects and a biological basis for the association must also be carefully examined.
Crucially, dietary intake of B vitamins influences the measurement of homocysteine, and dietary differences must therefore be considered when comparing populations with MTHFR variants.1 Lastly, both selection bias for patients who have been tested for MTHFR variants and ascertainment bias in retrospective cohorts may play a large role in influencing study results.
The most common MTHFR SNPs in the general population are the C677T (rs1801133) and A1298C variants (rs1801131), thought to affect the thermostability of the methylenetetrahydrofolate reductase.6 The C677T allele has been better studied, and its combined heterozygous and homozygous incidence varies from 20% to 30% in East Asian people to 20% to 40% in white and Hispanic populations in the United States.7 The A1298C variant is less well-studied, and its allele frequency is estimated at 10% to 30% in white populations and 20% to 40% in Southeast Asian populations (combined heterozygous and homozygous incidence).8 This variant is thought to be milder and less clinically significant.6
Advertisement
As mentioned, while these SNPs are associated with reduced methylenetetrahydrofolate reductase enzyme activity and increased homocysteine levels, the relationship between these findings and thrombotic risk has been controversial. Of note, homocysteine levels are impacted by many factors, including concomitant renal disease, thyroid disease, nutritional deficiencies and alcohol intake.1,9
Early analyses of whether homocysteine levels are associated with VTE came from a 1997 meta-analysis that pooled results of nine studies and showed an increased risk of VTE in the setting of hyperhomocysteinemia.10 A larger-scale meta-analysis comprising 11,000 cases and 21,000 controls from 31 databases was published in 2013. It showed that there was no evidence for an association with homozygotes for the MTHFR C677T variant and VTE, but due to incomplete data, was unable to examine for an association between homocysteine, MTHFR variant and VTE.11
Likewise, a review of nine case-control studies involving 382 patients found insufficient evidence to support any association between the MTHFR C677T variant and cerebral venous sinus thrombosis.12 A meta-analysis of 26 studies examining the role of the MTHFR C677T variant and recurrent unexplained pregnancy loss showed an association only in five studies from China and no association in European studies.13 The authors concluded that at most, the presence of this SNP is a risk factor for recurrent unexplained pregnancy loss in Chinese patients but not in European patients.13
Advertisement
Given the tenuous associations identified in the literature associating MTHFR variants with VTE, we do not advocate for the routine testing of patients for MTHFR variants. This approach is supported by the American College of Medical Genetics and Genomics.14
If a patient has had a prior genetic test with a result reported for MTHFR, the clinician must carefully consider whether the reported genetic change (whether it is an SNV, SNP, or more complex alteration) is known to be pathogenic and is consistent with the patient’s presentation. In cases where the identified genetic change is a common SNP, we do not recommend any further workup or management based on the prior genetic testing. In situations with rarer variants or complex genomic rearrangements identified, consultation with a genetic counselor may be helpful.
The propensity to clot is influenced by a myriad of factors in each patient, and a patient’s MTHFR status is a single, likely noncontributory component of this risk. In patients with VTE, the management of a patient with an MTHFR variant should be no different than the standard of care. In those who are at risk of thrombosis, it is essential to recognize that the common MTHFR SNPs are not thought to be contributory to VTE risk. Other risk factors such as age, family history, and medical comorbidities such as diabetes and hypertension are greater determinants of VTE risk. We recommend that all patients maintain a healthy weight, stop smoking, limit alcohol consumption and exercise regularly. Dietary modifications, such as including folate-rich foods like leafy greens, legumes, and fortified cereals, may also be beneficial.
Advertisement
The relationship between MTHFR variants and thrombosis risk is a complex, multifactorial issue. Early studies reported a potential association between common SNPs in MTHFR and VTE, but later, larger meta-analyses have refuted these results. At this time, based on the best available evidence, there is no support for the association of the most common MTHFR SNPs with significantly elevated thrombotic risk. We recommend that clinicians focus on modifiable risk factors of thrombosis, such as weight management, smoking cessation, and underlying medical issues.
This article is republished from Cleveland Clinic Journal of Medicine November 2023, 90 (11) 661-663.
1. Selhub J. Homocysteine metabolism. Annu Rev Nutr 1999; 19:217–246.
2. Frosst P, Blom HJ, Milos R, et al. A candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductase. Nat Genet 1995; 10(1):111–113.
3. Weisberg I, Tran P, Christensen B, Sibani S, Rozen R. A second genetic polymorphism in methylenetetrahydrofolate reductase (MTHFR) associated with decreased enzyme activity.
4. Govindaiah V, Naushad SM, Prabhakara K, Krishna PC, Radha Rama Devi A. Association of parental hyperhomocysteinemia and C677T methylene tetrahydrofolate reductase (MTHFR) polymorphism with recurrent pregnancy loss. Clin Biochem 2009; 42(4–5):380–386.
5. Firth HV, Hurst A. Oxford Desk Reference: Clinical Genetics and Genomics. 2nd ed. Oxford, United Kingdom: Oxford University Press; 2017.
6. Moll S, Varga EA. Homocysteine and MTHFR mutations. Circulation 2015; 132(1):e6–e9.
7. Wang X, Fu J, Li Q, Zeng D. Geographical and ethnic distributions of the MTHFR C677T, A1298C, and MTRR A66G gene polymorphisms in Chinese populations: a meta-analysis. PLoS one 2016; 11(4):e0152414.
8. Sherry ST, Ward MH, Kholodov M, et al. dbSNP: the NCBI database of genetic variation. Nucleic Acids Res 2001; 29(1):308–311.
9. Zhang Y, Wang Q, Li Q, Lu P. Association between hyperhomocysteinemia and thyroid hormones in euthyroid diabetic subjects. BioMed Research International 2015; 2015.
10. Ray JG. Meta-analysis of hyperhomocysteinemia as a risk factor for venous thromboembolic disease. Arch Intern Med 1998; 158(19):2101–2106.
11. Simone B, De Stefano V, Leoncini E, et al. Risk of venous thromboembolism associated with single and combined effects of factor V Leiden, prothrombin 20210A and methylenetethraydrofolate reductase C677T: a meta-analysis involving over 11,000 cases and 21,000 controls. Eur J Epidemiol 2013; 28(8):621–647.
12. Gouveia LO, Canhão P. MTHFR and the risk for cerebral venous thrombosis—a meta-analysis. Thromb Res 2010; 125(4):e153–e158.
13. Ren A, Wang J. Methylenetetrahydrofolate reductase C677T polymorphism and the risk of unexplained recurrent pregnancy loss: a meta-analysis. Fertil Steril 2006; 86(6):1716–1722.
14. Hickey SE, Curry CJ, Toriello HV. ACMG practice guideline: lack of evidence for MTHFR polymorphism testing [published correction appears in Genet Med 2020]. Genet Med 2013; 15(2):153–156.
Advertisement
Pinpointing how tumors reprogram platelets and trigger blood clots

IV thrombolysis should not be delayed because of planned thrombectomy

Multi-site study reveals surprising findings

Aim is for use with clinician oversight to make screening safer and more efficient

Genetic variants exist irrespective of family history or other contributing factors

CD36 loss-of-function variant accounts for large portion of risk in this population

First-in-human phase 1 trial induced loss of function in gene that codes for ANGPTL3

Paired blood and brain tissue methylation findings raise prospect of noninvasive precision diagnosis