Cutaneous complications common post-transplant
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
As use of lung transplant (LT) becomes more common, pulmonologists should be aware of post-transplant dermatologic complications. In a recent pictorial review in CHEST, my colleagues and I describe the pathogenesis, epidemiological characteristics and clinical manifestations of dermatologic complications found in lung transplant recipients. Here I will focus on Kaposi sarcoma.
Kaposi sarcoma are endothelial cell tumors often but not always associated with human herpes virus (HHV)-8 and generally classified into four subtypes based on clinical circumstances. Upon immunosuppression, especially with calcineurin inhibitors, HHV-8 can reactivate, proliferate and produce Kaposi sarcoma. Viral transmission can also occur during transplant. Use of mammalian target of rapamycin (mTOR) inhibitors can reduce the incidence of Kaposi sarcoma.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e62008fc-e7da-4338-a2c5-8320060a49fe/19pul075-fig-1_650x450_jpg)
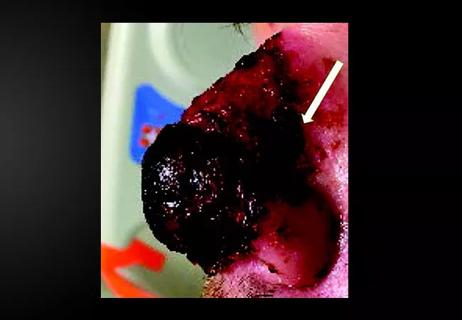
Note the woody induration and violaceous papules.
Kaposi sarcoma macules, plaques and nodules typically involve the skin or mucosa and appear purplish, dark brown or reddish blue and bleed and ulcerate easily. Post-transplant Kaposi sarcoma is typically more diffuse.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2bbda8e6-1393-449d-b491-4452f60d66e3/19pul075-fig-2_550x300_jpg)
Kaposi sarcoma in the right foot.
Kaposi sarcoma can be disfiguring. It can also cause lymphedema, pain and secondary infection.
Preventing and treating Kaposi sarcoma in lung transplant recipients
Donor screening for HHV-8 is important for seronegative transplant recipients, and mTOR inhibitors should be considered for seropositive recipients. I urge any transplant pulmonologist to incorporate counseling, treatment, education and referral to appropriate specialists into their post-transplant visits. Early treatment for suspicious lesions is of the utmost importance, especially in this population.
Advertisement
Dr. Mehta is staff in Cleveland Clinic Respiratory Institute’s Department of Pulmonary Medicine and a fellow of the American College of Chest Physicians.
Images are republished with permission from CHEST. The pictorial review also examines other cutaneous complications in recipients of lung transplants, including actinic keratosis, herpes virus, malignant melanoma and post-transplant squamous cell carcinoma, among others.
Advertisement
Advertisement

Family history may eclipse sun exposure in some cases

Consider secondary syphilis in the differential of annular lesions

Persistent rectal pain leads to diffuse pustules

Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus

Low-dose, monitored prescription therapy demonstrates success

Antioxidants, barrier-enhancing agents can improve thinning hair