Immune toxicity remains a diagnosis of exclusion, and multidisciplinary collaboration remains the cornerstone for early diagnosis and treatment.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/1ff729c2-4e8d-4fe3-8326-8d597cbee360/690x380-Antibiotic-jpg)
Antibiotics
Written by Simon Mucha
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A 69-year-old man presented with fever, acutely altered mental status and seizure-like activity. He was admitted to our medical ICU with the presumed diagnosis of sepsis from meningitis and started on empiric antibiotics and acyclovir. His medical history was significant for metastatic melanoma, treated with combination immune checkpoint inhibitor (ICI) therapy with ipilimumab and nivolumab. The patient achieved a significant reduction of tumor burden since the initiation of ICI therapy but recently required a steroid taper for an episode of immune-mediated pneumonitis.
On arrival, the patient was febrile, tachycardic, hypotensive and profoundly encephalopathic. Lumbar puncture was performed and showed neutrophilic pleocytosis (47 nucleated cells, 81% neutrophils, 17% lymphocytes), elevated protein (144 mg/dL nl = 15-60mg/dL) and normal glucose. Systemic inflammatory markers were markedly elevated (CRP 14.0 (nl = <1mg/dl), Il-2: 4703.7 (nl 175.3-852.2 pg/mL), IL-6: 34.3 (nl <6 pg/mL) LDH: 996 U/L (nl = 135- 225 U/L)). Infectious workup, however, including CSF-, blood- and urine cultures as well as viral PCRs and extensive imaging, including whole body PET-CT remained negative.
Given negative infectious workup and persistently elevated inflammatory markers, and unchanged symptoms despite broad-spectrum antibiotics, his clinical presentation was thought to be consistent with cytokine release syndrome (CRS) and encephalopathy due to autoimmune meningoencephalitis.
After multidisciplinary discussion between ICU, oncology, neurology and infectious disease teams, treatment with pulse dose steroids were initiated. This resulted in a dramatic improvement of the patient’s mental status. However, fever, tachycardia and elevation of inflammatory markers continued, consistent with persistent CRS. IVIG and treatment with the Interleukin-6 receptor antagonist tocilizumab were added for this. The first dose of Tocilizumab led to rapid resolution of symptoms and a decrease in inflammatory markers. The patient was able to be transferred out of the ICU for ongoing oncology care. (Figure 1).
Advertisement
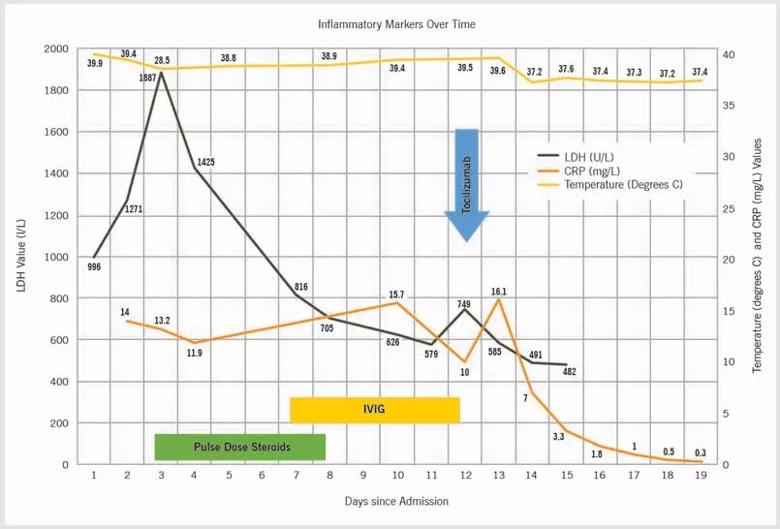
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7361a4e6-e06d-4258-a281-286ac6769cb5/22-PUL-3153114-CQD-Complex-Case-1-DrSimon-Mucha-805x546-1_jpg)
Figure 1. Steroids were started on Day 3 after admission, tocilizumab was given on Day 12 and IVIG was administered on Days 7-12. With the initiation of steroids, the patient saw a drop in LDH, persistent fevers, elevated CRP and clinical CRS. The patient’s fever and CRP resolved after tocilizumab.
Novel immunotherapies, such as ICIs, are revolutionizing modern oncology care. They are leading to durable responses and improved survival in many advanced cancers previously thought to be incurable. Despite improved outcomes, checkpoint inhibition is associated with a wide spectrum of unique immune-related adverse events (irAEs). Dermatologic, gastrointestinal, pulmonary and endocrine irAEs are most common, but virtually any organ system can be affected (Figure 2). Severe irAEs often mimic acute infections and sepsis and can progress to fulminant multi-organ failure without prompt recognition and aggressive anti-inflammatory treatment. As the use of ICI and other immunotherapies continues to grow, so will the number of patients hospitalized with potential therapy-related immune toxicity.
Recognizing the complexity of ICU care for patients with cancer and the importance of well-coordinated, interdisciplinary care, we have established a dedicated Oncology-ICU working group. Through continuous education, quality improvement and a daily virtual huddle that connects ICU and oncology specialists, this group of MICU nurses, advanced practice providers, pharmacists and physicians aim to facilitate timely, safe and effective care-specific ICU care. While CRS and severe neuro-toxicity are rare in ICI it is well described in cellular immunotherapy such as CAR-T cell therapy. Our prior experience in the use of steroids and IL-6 inhibitors in the treatment of CAR-T-associated CRS and neurotoxicity was essential to arrive at a timely diagnosis and develop and implement an effective treatment plan for this patient. This case highlights the complexity of immune-mediated toxicity associated with novel therapies and the importance of effective multidisciplinary ICU care.
Advertisement
Advertisement
Collaborative patient care, advanced imaging techniques support safer immunotherapy management
Highly personalized treatment shrinks tumors resistant to immunotherapy
Cleveland Clinic Cancer Institute among select group of centers to administer highly personalized treatment
Researchers develop first-of-its-kind neoantigen atlas to better understand immunotherapy resistance
Patients receive specialized inpatient and outpatient care for cellular, gene and immune cell-engaging therapies
Clinicians highlight the need to educate patients about warning signs
Benefits of neoadjuvant immunotherapy reflect emerging standard of care
Phase 2 trials investigate sitagliptin and methimazole as adjuvant therapies