Combo therapy shows longer OS and PFS and higher ORR
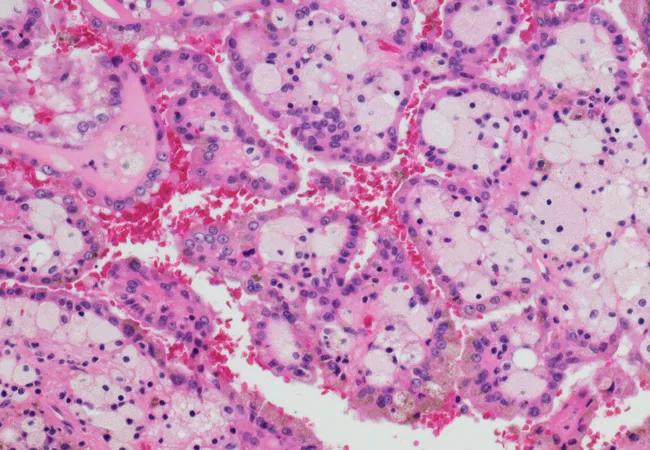
Since 2005, the advanced renal cell carcinoma (RCC) treatment landscape has undergone a major evolution: moving from cytokine-based immunotherapy, which achieved little clinical benefit, to targeted therapy against vascular endothelial growth factor (VEGF) and today to novel immunotherapy agents. As a cancer with immunogenic properties, RCC has responded well to immunotherapy. It has also proven susceptible to antiangiogenic treatment.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Enter KEYNOTE-426, a phase 3 trial comparing standard first-line anti-VEGF therapy sunitinib with a combination of two agents that have shown antitumor activity in previously untreated, advanced RCC: VEGF receptor tyrosine kinase inhibitor axitinib and anti-programmed death 1 (PD-1) monoclonal antibody pembrolizumab. Results were recently published in New England Journal of Medicine.
“These results mark another transition in the RCC treatment landscape. This is the first time a regimen has improved OS, PFS and ORR in an unselected front-line metastatic RCC population.” says Brian Rini, MD, Director, Genitourinary Program, Cleveland Clinic Cancer Center and principal investigator of the global trial. “Capitalizing on both an antiangiogenic and immunotherapeutic approach, benefit was seen across prognostic groups and regardless of PDL1 expression.”
The results of this open-label, randomized trial were staggering: the combination treatment resulted in a 47 percent lower risk of death and a 31 percent lower risk of disease progression or death compared with sunitinib treatment alone. The objective response rate in the pembrolizumab-axitinib arm was 59.3 percent (95% CI, 54.5-63.9) versus 35.7 percent in the sunitinib arm (95% CI, 31.1-40.4). Median progression-free survival was 15.1 months for the combination therapy and 11.1 months for sunitinib alone (HR for disease progression or death, 0.69; 95% CI, 0.57-0.84; P < 0.001).
Patients received either pembrolizumab (200 mg) intravenously once every three weeks plus oral axitinib (5 mg) twice daily (N = 432) or oral sunitinib (50 mg) once daily for the first four weeks of each six-week cycle (N = 429). Patients all had previously untreated advanced clear-cell renal cell carcinoma. Imaging was performed at week 12 and then every six weeks for the first year and every 12 weeks thereafter. Bone scans were performed at baseline and, when positive, repeated at weeks 18, 30, 42 and 54 and every 24 weeks thereafter. Adverse events were monitored throughout and graded per National Cancer Institute Common Toxicity Criteria for Adverse Events.
Advertisement
Eligible patients were treatment naive with histologically confirmed metastatic RCC with clear cell component (with or without sarcomatoid features), measurable disease (RECIST v1.1, investigator review), no prior systematic therapy for advanced disease and Karnofsky performance status greater than 70 percent.
As multiple frontline trials of checkpoint immunotherapy in combination with either targeted therapies or other checkpoint inhibitors are demonstrating promising results, there is newfound hope for patients with advanced RCC. “We’re seeing positive results in many trials, including KEYNOTE,” says Dr. Rini. “We are also finally starting to get larger numbers of advanced kidney cancer patients into remission. Clinical research will continue, however, until all metastatic kidney cancer patients can be cured.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors