20 years of data suggest that ablation is a valid treatment option
In select patients with multifocal, small neuroendocrine liver metastases (NELM) that occupy less than 20% of liver volume, laparoscopic ablation (LA) can result in effective local tumor control while improving quality of live and generating favorable oncologic outcomes, according to a study from Cleveland Clinic.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“To our knowledge, this is the largest single-center experience with LA for the treatment of NELM in the literature,” says Eren Berber, MD, Director of Robotic Endocrine Surgery, the Liver Tumor Ablation Program and the Neuroendocrine/Adrenal Tumor Center at Cleveland Clinic, and senior author on the study. “Additionally, with 20 years of cumulative data, we believe it represents the longest follow-up reported to date.”
Researchers analyzed retrospective data from patients who received ablation treatment for NELM from 1996 through 2018. All in, there were 129 patients with 770 NELMs who underwent 177 ablation sessions.
While most patients (N = 93) were treated in one session, several (N = 27) had two sessions, a handful (N = 7) had three sessions, one patient had four sessions, and one patient had five sessions. Radiofrequency ablation was most common (150 sessions), with microwave thermosphere ablation accounting for the remaining 27 sessions.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/7f2e386e-667a-4d22-8262-99f908e4cab5/2015F1-300x143_jpg)
MWA needle (A) and generator (B) used in the study. The needle is 30 cm, 13.5 G and the generator is 2.45 GHz. The system uses saline circulation to cool off the antenna. Reprinted by permission from Springer Nature: Berber E. Laparoscopic microwave thermosphere ablation of malignant liver tumors: an initial clinical evaluation. Surgical Endoscopy. 2016:30(2):692-698.

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/2db64dda-ca85-4fb1-9c5a-6823092b401b/2015F2-226x300_jpg)
Intraoperative photo showing the trocar placement for laparoscopic MWA. Two 12-mm trocars are used for the laparoscope and ultrasound probe. The microwave antenna is placed through a 3- to 5-mm trocar. The procedure is monitored in real time with laparoscopic ultrasound. Reprinted by permission from Springer Nature: Berber E. Laparoscopic microwave thermosphere ablation of malignant liver tumors: an initial clinical evaluation. Surgical Endoscopy. 2016:30(2):692-698.
Advertisement
LA is a minimally invasive approach that has low morbidity and seems to compare favorably to resection. However, Dr. Berber cautions that selection bias may be an issue, and many factors should be considered when selecting the right patients for LA.
At 6%, the complication rate was low and in line with previous reports. Most (92%) patients experienced hormonal symptom relief for a median of 25 months.
Median survival after LA was 125 months, with 1-year survival of 93%, 5-year survival of 76% and 10-year survival of 59%. Comparable to previously reported data, 5-year and 10-year progression-free survival rates following LA were 26% and 6%, respectively. Independent predictors of poor overall survival were high tumor grade, larger tumor size and the presence of a nonresected primary tumor.
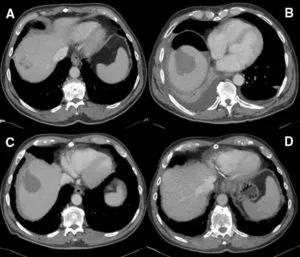
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/86d9965d-30ba-4ad7-99b1-723ebd2c6b52/Figure-1-300x257_jpg)
Computerized tomography images of a patient with 3 liver metastases A treated with laparoscopic radiofrequency ablation. Follow-up scans at 2 weeks (B), 3 months (C), and 10 years (D) confirm successful tumor destruction. Figures demonstrate the dominant lesion. Reprinted by permission from Springer Nature: Kose E, Kahramangil B, Aydin H, Donmez M, Takahashi H, Aucejo F, Siperstein A, Berber E. Outcomes of laparoscopic tumor ablation for neuroendocrine liver metastases: a 20-year experience. Surgical Endoscopy. 2020:34(1):249-256.
Thirty-three percent (N = 43) of patients had multiple residual tumors measuring < 1 cm, which were intentionally left untreated following ablation. Local recurrence rates were 5% per lesion and 22% per patient. Overall, during follow-up, 71% of the patients developed recurrent liver disease.
Advertisement
“At our institution, we have a strict follow-up protocol for patients like this with residual disease,” Dr. Berber continues. “For the first two years following ultrasound-guided liver ablation, patients are monitored quarterly with computerized tomography or magnetic resonance imaging. We follow them on an biannual basis after that. Our follow-up protocol allows us to identify local recurrence and progression early, enabling timely intervention.”
When residual tumors enlarge to 2 cm or hormonal symptoms recur, the team considers repeat therapies directed to the liver according to amount of liver volume involved:
“Most patients with NELM live a long time, making symptom control and quality of life important things to consider when planning treatment,” Dr. Berber concludes. “We undertook this analysis in order to illustrate our 20-year experience with LA. Given the low morbidity associated with this minimally invasive approach, our data suggest that LA be experienced surgeons is a valid option in select patients with less than 20% of liver volume involved.”
Advertisement
Advertisement
Clinical trials and de-escalation strategies
Combination therapy improves outcomes, but lobular patients still do worse overall than ductal counterparts
Bringing empathy and evidence-based practice to addiction medicine
Supplemental screening for dense breasts
Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors
Early results show strong clinical benefit rates
The shifting role of cell therapy and steroids in the relapsed/refractory setting
Radiation therapy helped shrink hand nodules and improve functionality