Long-term weight redistribution, low surgical risk and short operation time
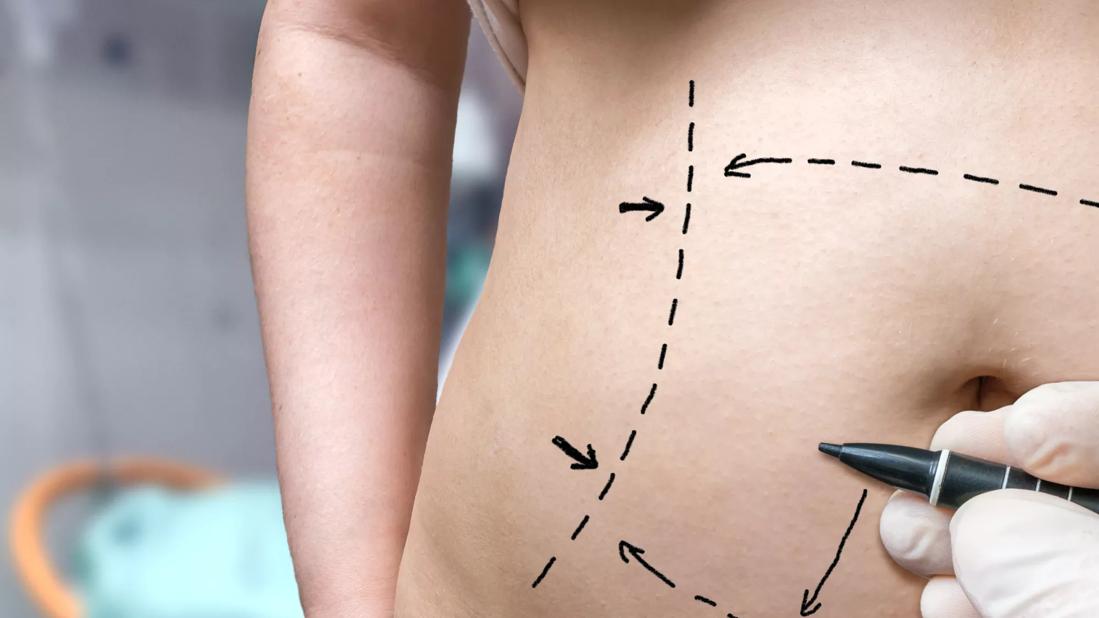
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/8c20d6de-2292-4cb1-b587-aa4f929c49cf/TummyTuck-scaled-jpg)
Liposuction
Shannon Wu, Demetrius M. Coombs, MD, and Raffi Gurunian, MD, PhD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Please note: This is an abridged version of an article originally published in the Cleveland Clinic Journal of Medicine.
Liposuction allows plastic surgeons to semipermanently redistribute volume in accordance with a patient’s ideal, and with lower complication, morbidity and mortality rates than with other surgical procedures. This article reviews common liposuction techniques and complications.
The era of modern liposuction began in 1975 when Arpad and Fischer pioneered the use of blunt hollow cannulas and suction curettage for liposuction on the outer thighs, but the patients ultimately experienced deforming lymphorrhea.7 An important milestone was reached in 1977 when Illouz developed the “wet technique,” in which injection of hypotonic saline solution and hyaluronidase into adipose tissue before liposuction reduced hemorrhagic risk.8 This type of hydrodissection, similar to that used today, preserved neurovascular bundles and enlarged the deep adipose layer for easier aspiration.
In 1983, Fournier used syringes instead of mechanical suction for better control of negative pressure.9 By 1987, Klein had developed the tumescent technique—a type of local anesthesia infiltration that permitted the removal of larger volumes of fat while reducing bleeding.10 Toledo expanded the use of syringes to include various gauges and sizes for aspiration of adipose tissue in 1988.11
In the early 1990s, the development of ultrasonographically guided liposuction by Zocchi expanded the use of liposuction for previously unfavorable, fibrous areas such as the buttocks.12,13 The development of minimally invasive, laser-assisted liposuction by Apfelberg, also in 1992, prevented destruction of neurovascular structures by cannulas and promoted tissue tightening for an aesthetic result.14 Recently, the development of power-assisted liposuction has further expanded and improved this procedure, increasing the popularity and use of liposuction.15
Advertisement
Suction-assisted lipectomy: Negative pressure from a syringe applied to a small-volume, blunt-tip suction cannula is used to remove fat.29 Suctioning from the superficial layer should be avoided to prevent dimpling, hyperpigmentation, and contour irregularities.19 The superficial fat layer contains vertical fibrous septa, which would result in contour deformities if disrupted; however, exploitation of this anatomy with the liposuction cannula, also known as abdominal etching, has been demonstrated to produce highly defined abdominal aesthetic contours (e.g., “6-pack abs”).33
Ultrasound-assisted lipectomy: Transmitting ultrasound energy to emulsify fat prior to its removal,34 ultrasonographically assisted lipectomy (UAL) can be advantageous in fibrous areas, such as the back, chest and upper flank, that are more difficult to target in standard liposuction. UAL has shown marked benefit in treatment of gynecomastia. However, larger incisions are required in UAL and operations require more time. There is an increased risk of thermal injury to subdermal tissues due to the exothermic energy caused by ultrasound.
Laser-assisted lipectomy: Laser-assisted lipectomy (LAL) is performed by inserting a laser fiber via a small incision.35 Although complications of LAL are rare, one study observed a complication rate of 0.93% that included skin burns and a local infection.36
Power-assisted lipectomy is performed with an external power source, typically an electric vacuum pump.35 This technique can be advantageous for large volumes of tissue removal and in densely fibrous areas, as the power assistance reduces operator fatigue.
Advertisement
The most common technique remains the traditional suction-assisted lipectomy.33–36 Small-volume liposuction procedures in which a maximum of 1,000 mL of fat is removed can be performed with local anesthesia. Although there is no maximum volume of fat that can be removed in a single setting, the risk for seroma and fluid imbalance increases along with the volume of fat that is removed.
Megaliposuction, a procedure in which an amount greater than 10% of body weight is removed, can be safely performed by an experienced surgeon. Large-volume liposuction procedures should be performed with general anesthesia.19 Harvested fat may be used for subsequent fat transfer.19
The advantages of liposuction are short surgery time (typically under three hours, depending on the extent of fat removal) and concomitant procedures. In addition, patients undergoing liposuction have a short recovery period, unobtrusive scars, permanent results, low complication rates, and low morbidity and mortality rates relative to other surgical procedures. Because adipocytes are removed, further storage of fat in those areas is limited, leading to high patient satisfaction with long-term results.37
More research is needed to determine the degree of fat reaccumulation in the treated area and redistribution to nontreated areas.38,39 As expected, weight gain can still occur, and the patient should be advised to maintain a well-balanced diet and exercise regimen.
Complications are relatively uncommon in liposuction and of low risk relative to other procedures.42 In one study, the overall complication rate was 2.4%.43 The complication rate was higher (3.5%) when liposuction was combined with other procedures, whereas liposuction as a solitary procedure had a complication rate of only 0.7%.41 Complications include ecchymosis, edema, surgical site infection, seroma, hematoma and venous thromboembolism.43
Advertisement
The most common complication of liposuction is contour deformity. As many as 9% of patients may report soft-tissue depressions or elevations, skin panniculus, folds, or wrinkles.44 Contour deformities can be prevented by using smaller diameter cannulas, avoiding suctioning from superficial layers, employing a “crisscrossing” technique, and allowing slight undercorrection for postoperative fat lysis.45 Seroma and hematoma are also rare complications of liposuction.46 Seromas, which are collections of serous fluid resulting from breakdown of the fibrous tissue network, may develop from initial blind cannula injury to small perforating vessels or lymphatic vessels.31 Use of progressive tension sutures—primarily a technique to address dead space in surgeries such as abdominoplasty (“tummytuck”)—has been shown to reduce the rate of seroma from 9% to 2%.46 Wound infection is reported in fewer than 3% of inpatient liposuction cases and in approximately 1% in outpatient surgeries.47 Low infection rates can be attributed to surgeon expertise, proper prophylactic antibiotics, and sterile technique, among other factors.
Although uncommon, early-stage wound infections (i.e., cellulitis) may develop into more severe sepsis or necrotizing fasciitis—the latter of which is a surgical emergency.48 A 2018 study estimated that after liposuction with or without subsequent fat grafting, at least 17 patients have experienced clinically significant fat embolization, or fat embolization syndrome.49 However, more recent data suggests that worldwide, fatal and nonfatal fat embolism, particularly after gluteal fat grafting, may exceed 135 cases.50
Advertisement
Although fat embolism is rare, its mortality rate of 10% to 15% warrants careful postoperative monitoring for rapid detection and treatment, and it has been reported to occur within 12 to 72 hours after surgery.50,51 As described, gluteal fat transfer is the only procedure with a higher risk of fatal fat embolism, and is still considered to have the highest mortality rate of any aesthetic procedure.52 The incidence of venous thromboembolic events (deep venous thrombosis and pulmonary embolism) after liposuction is low at 0.03%.53,54
Pulmonary embolism is the most common cause of death after this procedure, which carries an overall mortality rate of 0.01%.54 Sameday ambulation after liposuction surgery is encouraged to prevent thromboembolic events. As with any surgical procedure, liposuction causes a transient elevation of acute inflammatory markers (interleukin 6, C-reactive protein), but there is no increased risk of progression to renal disease or chronic inflammation.55
Some studies suggest that, due to permanent removal of adipocytes, the long-term metabolic benefits of liposuction include improved insulin sensitivity and reduced inflammation. However, more studies are warranted.56 Systemic complications that arise weeks to months after surgery include edema, lymphedema, wound dehiscence, hypertrophic scar formation, ecchymosis and skin laxity. Blind cannula injury can lead to abdominal wall injury, bowel perforation or vessel injury. Although uncommon, skin devascularization and skin necrosis can occur if the surgeon suctions too closely to the skin undersurface and injures the dermal plexus.57
Breast augmentation with autologous fat transfer may lead to fat necrosis that mimics microcalcifications suspicious for breast cancer on mammographic imaging.58 However, the incidence of these imaging findings is similar to those in patients without fat transfer, and thus, breast augmentation does not hinder detection of breast cancer.
Liposuction can improve body contour and reduce body mass index, and advances are continually being developed. Due to the benefits of long-term weight redistribution, low surgical risk and short operation time, patients seeking body contour changes will continue to pursue liposuction. The long-term effects on metabolic sequelae such as insulin sensitivity are still being actively researched.59,60
Noncosmetic indications are also expanding, particularly fat grafting for breast, facial and pedal reconstruction.61 Although liposuction can address a wide variety of needs spanning from cosmetic to reconstructive purposes, the procedure is rarely covered by Medicare or third-party insurance plans, even for issues that cause functional impairment.62 Research is being performed in noninvasive body contouring such as cryolipolysis, which may decrease subcutaneous fat deposits while providing dermal tightening with no surgical scars.63,64
Note: For complete references, please visit the Cleveland Clinic Journal of Medicine.
Advertisement
Family history may eclipse sun exposure in some cases
Consider secondary syphilis in the differential of annular lesions
Persistent rectal pain leads to diffuse pustules
Two cases — both tremendously different in their level of complexity — illustrate the core principles of nasal reconstruction
Stress and immunosuppression can trigger reactivation of latent virus
Low-dose, monitored prescription therapy demonstrates success
Antioxidants, barrier-enhancing agents can improve thinning hair
A hybrid approach