A case report from the hepatopancreaticobiliary clinic
By Mujtaba Mubashir, MD, and R. Matthew Walsh, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
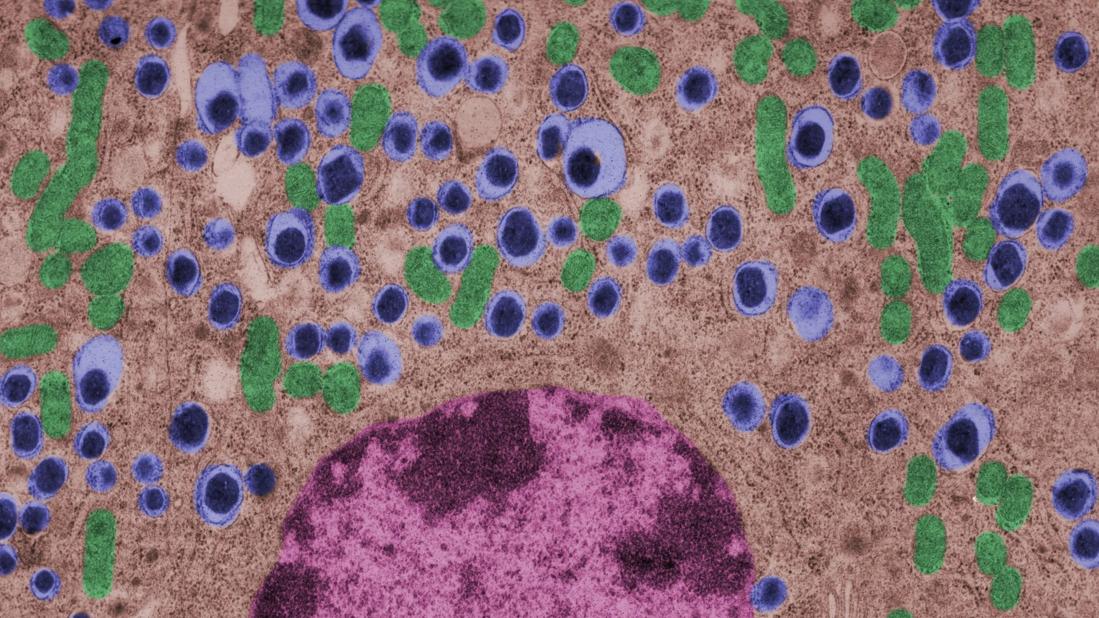
Chronic pancreatitis causes severe disability for most patients. A last resort aimed at alleviating symptoms of pain for these patients is a total pancreatectomy, a complex procedure that can result in a host of issues including the development of iatrogenic diabetes due to the loss of insulin producing islet cells. One solution is autotransplanting islet cells from a patient’s explanted pancreas by introducing the cells into the portal venous system. The cells ultimately implant into the liver and theoretically alleviate the problem of diabetes following remove of the pancreas.
Hepatopancreaticobiliary (HPB) surgeons at Cleveland Clinic performed their first total pancreatectomy with islet cell autotransplantation in 2007 and since then has become one of the world’s largest centers for performing this complex procedure in all age groups. Several Cleveland Clinic studies have shown outcomes similar to other high-volume centers, including centers that harvest islet cells onsite.
Some of the cases that we have encountered at the Cleveland Clinic requiring this procedure are particularly unique. The following is a case of a young male with Byler disease who required liver transplant followed by total pancreatectomy and islet cell autotransplant for debilitating episodes of pancreatitis.
Byler disease, or progressive familial intrahepatic cholestasis (PFIC), is an autosomal recessive condition that was first described in the Amish population. It usually manifests in infancy and leads to progressive cholestasis, failure to thrive and ultimately a need for liver transplant.
Advertisement
Our patient was diagnosed with PFIC-1 at five weeks of age given presence of the same condition in his older brother. Symptom onset was at about two months of age, when he developed cholestasis and failure to thrive leading to the development of rickets. In October 2005, he underwent a partial biliary diversion with retro-colic hepaticojejunostomy with Roux ostomy with subsequent resolution of his jaundice.
He then established care at Cleveland Clinic and was followed closely by the pediatric gastroenterology team at regular intervals. He continued to do well, did not experience any significant gastrointestinal issues, and had a healthy appetite, normal bowel function and appropriate growth curve.
At the age of 12, he was admitted with severe cholestasis after being treated with penicillin for a finger laceration. This resulted in extremely high bilirubin and pruritus (total and direct bilirubin 31.5 and 20.7, respectively). Liver biopsy showed findings of Byler disease but also increased cellularity, possibly consistent with drug-induced cholestasis. He was admitted later that year with multiple episodes of pancreatitis and cholestatic jaundice, with increasing hyperbilirubinemia, pruritus, poor appetite, fat malabsorption and weight loss. He was thus considered a candidate for liver transplantation for a MELD (Model for End-state Liver Disease) exception of 30 and poor quality of life.
In January 2018, the patient underwent an orthotopic liver transplantation using the left lobe from a split liver with hepaticojejunostomy, biliary drainage and no bypass. He also underwent excision of the efferent loop of his existing biliary diversion to the skin stoma. After an uneventful postoperative course, he was discharged; however, he was soon readmitted with abdominal pain, diarrhea, jaundice, transaminitis, pleural effusion requiring chest tube, ascites requiring peritoneal drain, and transplant rejection (both acute cellular and antibody-mediated rejection) requiring antirejection course including steroids, intravenous immunoglobulin, rituximab and anti-thymocyte globulin.
He developed several episodes of recurrent acute pancreatitis requiring multiple hospitalizations, with five bouts in 2018 post-transplant, seven bouts in 2019 and four bouts in 2020. He was referred to the HPB clinic for further evaluation and was determined to be a candidate for total pancreatectomy with islet cell autotransplantation.
Advertisement
In June 2020, he underwent an exploratory laparotomy and spleen-preserving total pancreatectomy followed by pancreatic islet cell autotransplantation that same evening. During this operation, an extensive lysis of adhesions was performed, followed by a total pancreatectomy with sparing of the spleen and reconstruction with a gastrojejunostomy using the Roux limb proximal to the existing hepaticojejunostomy. The pressures in the portal vein into his liver transplant were very high which did not allow infusion of all the islets into the liver. Roughly half were randomly distributed in the abdomen for implantation on the peritoneal surface.
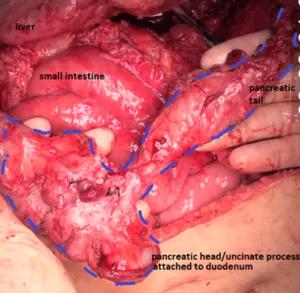
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d37436cd-89db-4895-9a70-ba98e78544f4/walsh-inset-300x293_png)
Excised pancreas, with head/uncinate process on bottom left attached to duodenum and pancreatic tail in top right.
Postoperatively, he had acute clinical deterioration with worsening respiratory status in setting of acute respiratory distress syndrome requiring reintubation, acute kidney injury (AKI) in the setting of supratherapeutic antirejection medications, prominent ascites requiring peritoneal drain placement twice, and development of multifocal pneumonia that subsequently improved. Liver function remained normal throughout this time, and excellent glycemic control was achieved. He was initially on tube feeds and was gradually advanced to an oral soft diet which he tolerated well.
He was ultimately discharged after adequate pain control, optimization of glycemic regimen, resolution of AKI and pneumonia and optimization of immunosuppressive regimen. He has since been seen in the outpatient setting and has progressively improved, including better tolerance of diet, resolution of pain, good glucose control and improved functional status compared with presurgical status. The HPB clinic continues to monitor his care.
Advertisement
To refer a patient to the HPB clinic, call 855.733.3712.
Dr. Mubashir is a general surgery resident. Dr. Walsh is Interim Chair of the Digestive Disease & Surgery Institute.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years