Participants overwhelmingly positive about their surgery

By Marsha Kay, MD, and Tracy Hull, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
For pediatric patients with ulcerative colitis, management of the disease is important for both controlling symptoms and preventing negative consequences such as malnourishment that can hamper growth and development. When medical management fails to relieve symptoms or there is a risk of dysplasia (precancerous changes in the lining of the colon), surgery is an effective option.
The surgery of choice is proctocolectomy with ileal pouch anal anastomosis (IPAA). This procedure removes the colon and rectum and creates a pouch from the ileum to hold stool. Pouch types include the more common J-pouch, which is easier to construct, and the S-pouch, which is used for patients with anatomical challenges and is technically more demanding to construct.
Research has been limited on long-term outcomes of IPAA in pediatric patients. To learn more about how patients fare over time and to have more data to guide surgical decisions, the Departments of Pediatric Gastroenterology and Colorectal Surgery conducted a study on long-term surgical outcomes in pediatric patients who were treated at Cleveland Clinic, which performs more surgeries for ulcerative colitis (UC) than any institution in the world.
The study surveyed 157 pediatric surgical patients who underwent IPAA from 1982 to 1997 and participated in an initial follow-up survey in 2002. The most common indication for surgery was failure of medical management. We reached 74 patients, with a median age of 38 years (39 male and 35 female) and a median age at surgery of 18 years, making it the largest and longest follow-up study in pediatric patients to date.
Advertisement
Participants reported a variety of complications over the average 20-year time period following the surgery; the most common was pouchitis (inflammation of the pouch), which was reported by 45 percent of participants. This condition is a well-known and common complication of pouch procedures occurring in patients of all ages, with a known increase in frequency with longer term follow-up. Pouchitis is primarily treated with medical therapy, and patients are usually able to retain their pouch.
Other complications included fistulae (30 percent), strictures (16 percent), obstruction (20 percent), pouch failure (14 percent) and change of diagnosis to Crohn’s disease (28 percent). More female patients than male patients reported obstruction, which may be due to anatomical differences. Pouch failure was significantly associated with a change in diagnosis to Crohn’s disease and having an S-pouch. However, most patients (60 percent) later diagnosed with Crohn’s disease were able to keep their pouch. None of the participants reported the development of dysplasia.
Fertility issues are a potential concern for women with inflammatory bowel disease (IBD) who undergo IPAA — infertility rates for this group are two to three times higher than for women with IBD who are treated with medical management. In our study, half of the 21 women who had children reported having some difficulty during pregnancy or difficulty conceiving, but the survey data did not analyze the specific issues involved. No males in the study reported fertility issues.
Advertisement
At follow-up, nearly half of the participants reported taking medications to control stooling frequency, which increases with an IPAA procedure, and 19 percent were on antibiotics, which is the initial treatment of choice for pouchitis. Some of the patients were on biologics and immunomodulators at follow-up, likely reflecting the group that had a change in diagnosis to Crohn’s disease with long-term follow-up.
Despite the complications, participants were overwhelmingly positive about their surgery: 79 percent were very satisfied and 14 percent were somewhat satisfied with how they were doing at long-term follow-up.
Over the past two decades, there have been significant advances in the diagnosis and treatment of UC. We use the latest technologies such as wireless capsule endoscopy and MRE (magnetic resonance enterography) to aggressively evaluate the small intestine and better distinguish between UC (which does not involve the small intestine) and Crohn’s disease, so that patients can receive the appropriate treatment for their condition.
New medications, such as the biologic agents infliximab and adalimumab (initially available in 1998 and 2002, respectively), have dramatically improved quality of life for UC patients and have significantly decreased the need for surgery.
Surgical techniques have also advanced: IPAA can be performed laparoscopically, which shortens recovery time and reduces scar tissue, potentially making infertility less of an issue for women. We are able to construct J-pouches in more patients, which reduces the chances of pouch failure. We also are better able to manage complications during the perioperative period, which may reduce the incidence of long-term complications. Cleveland Clinic pediatric gastroenterologists and colorectal surgeons work as a team to evaluate patients and select appropriate candidates for surgery. Our patients who have had IPAA procedures have done very well.
Advertisement
Patients with UC who are diagnosed and aggressively treated during the early stage of their disease typically achieve better outcomes due to earlier initiation of medical therapy, although some patients with severe disease at onset may still require surgery. Pediatricians should be alert to possible UC symptoms such as abdominal pain, diarrhea including nocturnal bowel movements and fecal urgency, blood in stools, weight loss, and unexplained fevers, especially if there is a family history, and refer patients for a consultation with a pediatric gastroenterologist.
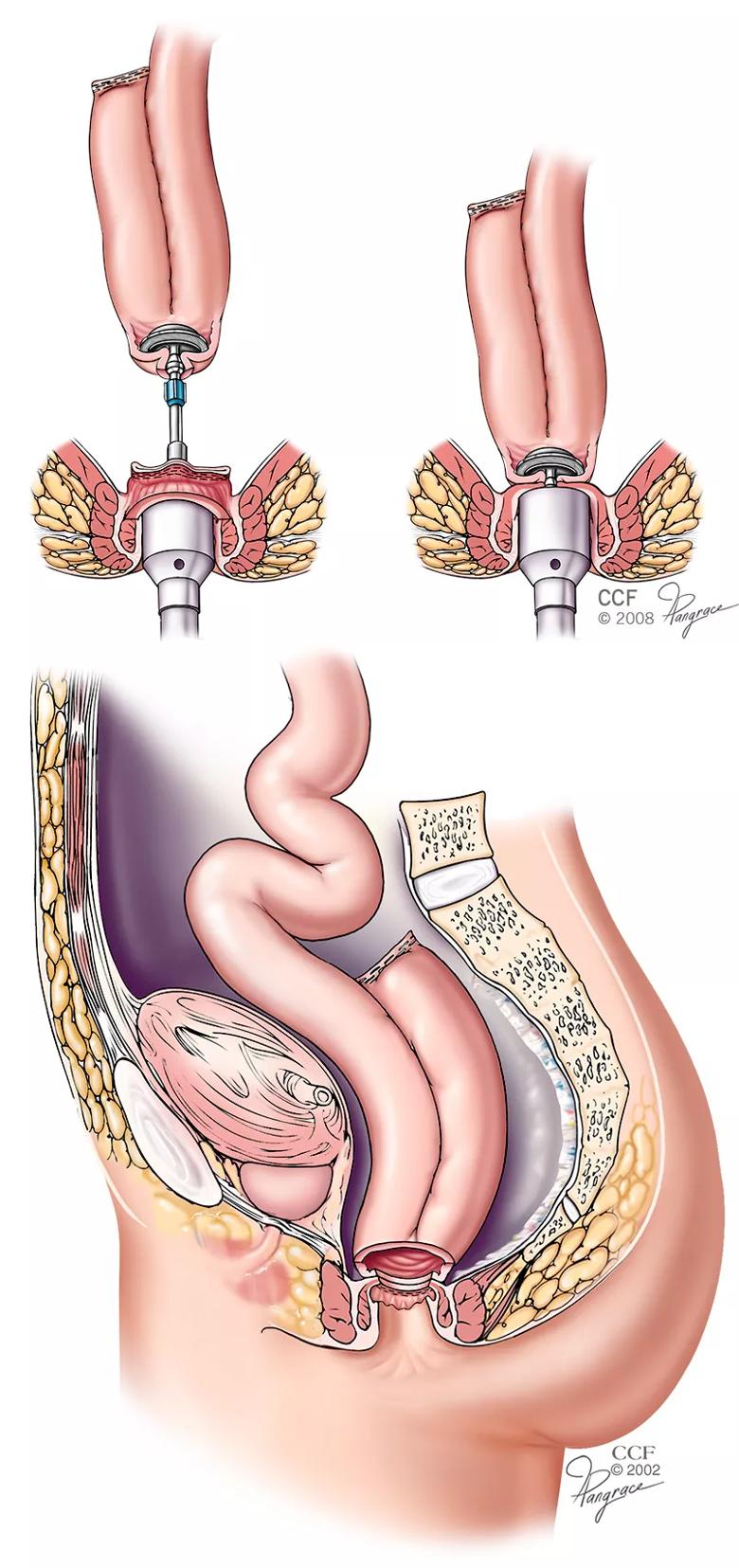
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e2889157-fca0-4c05-907b-e353d65d935c/650x450-J-Pouch_jpg)
Figures 1 & 2. A J-pouch is constructed using two loops of small intestine measuring approximately 6 inches in length. After pouch construction is complete, the pouch is capable of holding about two-thirds of a pint of fluid. The pouch is filled with sterile saline to ensure it is completely watertight. After testing, the pouch is placed into the pelvis where the rectum used to be and attached to the upper portion of the anal canal. This is the primary pouch procedure done at Cleveland Clinic.
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years