Findings support the safety of the technique
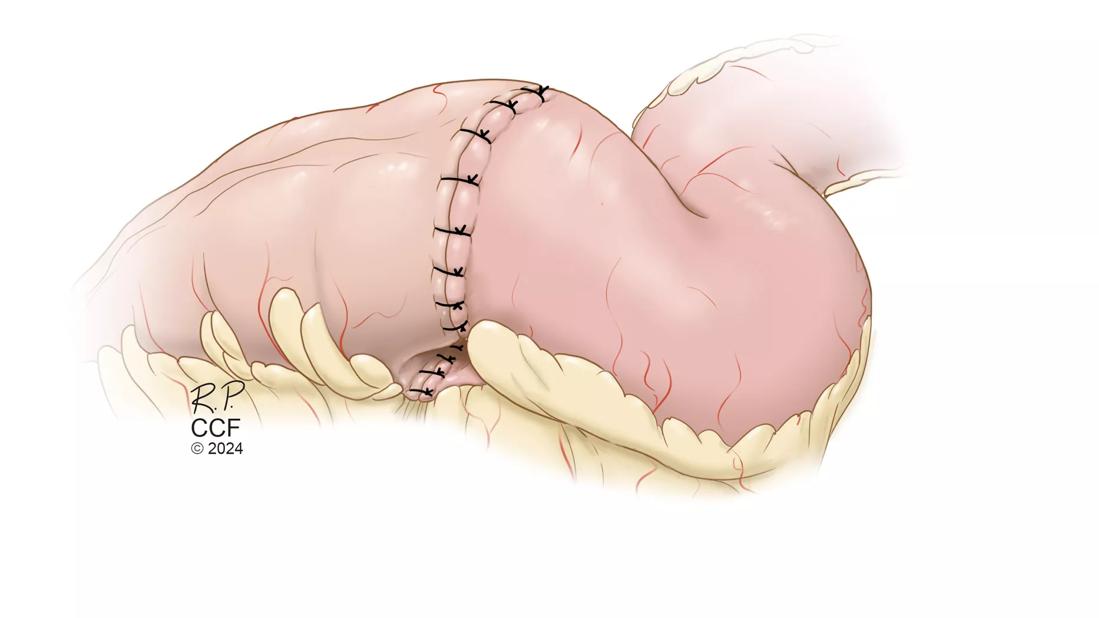
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5c8d130b-5017-4d25-b1dc-227c917e8bf3/kono-s-ileocolonic-anastomosis-crohns)
Medical illustration of Ileocolic Resection
A recent research effort at Cleveland Clinic, which compared Kono-S anastomosis and stapled side-to-side (SSTS) anastomosis in patients with Crohn's disease, showed no statistically significant difference in overall long-term recurrence-free survival between the two approaches.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
However, the analysis demonstrated that Kono-S anastomosis was independently associated with a decreased rate of endoscopic or surgical intervention for perianastomotic recurrence among the study population.
“Ileocolic resection and anastomosis is the most common intestinal operation for Crohn's disease,” says study author Stefan Holubar, MD, IBD Surgery Section Chief and Director of Research, Department of Colorectal Surgery, Cleveland Clinic, while also noting that the choice of anastomosis remains a topic of debate.
The SuPREMe-CD study (NCT02631967), the first randomized controlled trial to compare Kono-S and standard anastomosis among patients with Crohn's disease, demonstrated a reduction in postoperative endoscopic and clinical recurrence rates for patients who underwent Kono-S anastomosis. However, Dr. Holubar notes that additional studies have since been released that suggest Kono-S anastomosis did not have a protective effect.
“This debate is a hot topic because the mesentery has recently been implicated in the pathophysiology of Crohn's disease recurrence,” says Dr. Holubar, whose team set out to better understand Kono-S and its impact on patient outcomes. “Surgeons are trying to use surgical methods which target the mesentery to see if we can influence the natural history and decrease the risk of recurrence for these patients so that they can avoid having to undergo repeated surgeries in the future.”
The poster was presented at the annual 2024 European Crohn’s and Colitis Organisation Congress in Stockholm, Sweden.
Advertisement
Dr. Holubar and colleagues hypothesized that Kono-S anastomosis was associated with a lower risk of postoperative recurrence requiring intervention when compared to stapled side-to-side anastomosis.
Their analysis included consecutive patients from a prospectively maintained database who underwent ileocolic anastomosis for terminal ileal Crohn’s disease between 2020 and 2022. Patients with other types of anastomoses were excluded from the study.
The research group compared short-term postoperative outcomes and interventions for perianastomotic recurrence between the Kono-S and stapled side-to-side anastomosis. “We prospectively performed these procedures and then conducted a retrospective review, including long-term follow-up, to see what the endoscopic and clinical recurrence was, either requiring surgery or endoscopic reintervention, specifically, endoscopic balloon dilation,” Dr. Holubar explains.
Overall, 174 patients underwent ileocolic anastomosis. Of those, there were 83 patients (47.7%) in the Kono-S anastomosis group and 91 (52.3%) in the side-to-side anastomosis patient cohort. When compared to SSTS, median BMI was lower (24.3 vs. 26.4 kg/m2, P = .04), median operative time was longer (186 vs. 146 minutes, P < .001), and there was more mesenteric excision (53% vs. 15.4%, P < .001) among patients who underwent Kono-S anastomosis.
Dr. Holubar and colleagues observed no significant differences in short-term postoperative outcomes between the two groups. After 12 months, endoscopic recurrence developed (with a Rutgeerts score ≥ i2, P = .81) in 12 (30%) patients in the Kono-S cohort and 14 (35%) in the SSTS group, they reported.
Advertisement
“Compared with the SSTS group, the Kono-S group received more post-operative biologics (65.1% vs. 39.6%, P = .001) and more frequent medical therapy for perianastomotic recurrence (18/20 (90%) vs. 15/22 (68%); P = .14),” according to the study authors. “On multivariable analysis, Kono-S was associated with a significantly lower risk of perianastomotic recurrence requiring surgical and endoscopic intervention (OR 0.09, 95% CI 0.01-0.95, P =.05).”
Additionally, the analysis supports the safety of Kono-S anastomosis, with no increased risk of complications reported.
In summary, the researchers did not observe a difference in endoscopic postoperative recurrence, specifically looking at the Rutgeerts score, between Kono-S anastomosis and SSTS. “However, what we did find was that Kono-S seemed to be protective for surgical or endoscopic intervention for perianastomotic recurrence,” says Dr. Holubar. “This major finding of the study suggests that Kono-S anastomosis has a benefit for these patients.”
Moving forward, Dr. Holubar and colleagues continue to gather data from these patients and explore this area of study. “The overlying discussion is the role of the mesentery in ileocolic Crohn's disease and the other procedure we use pretty liberally because it has been shown to be safe, is extended mesenteric excision,” he says.
“In the current study, we found that the mesenteric excision did not add anything above and beyond the protection provided by the Kono-S anastomosis,” he adds. “We have another cohort of patients who have undergone mesenteric incision without Kono-S, and we are actively reviewing the medium- and long-term outcomes for these patients as well.”
Advertisement
Dr. Holubar concludes, “IBD surgery is a subspecialty within colorectal surgery and Kono-S anastomosis continues to be a hot topic that is still open for debate. The world is waiting for multiple, large, multicenter randomized trials, but my takeaway is that we cannot just look at the short-term outcomes. We really need to look at the long-term outcomes to determine if this is something that we should add routinely to our armamentarium of surgical options for these patients.”
Advertisement
Advertisement
Study utilizes prospective data from the RISK cohort
Nationwide research underscores the importance of individualized treatment
Strong patient communication can help clinicians choose the best treatment option
Findings from a 2023 ASCRS presentation indicate that both 2-stage and modified 2-stage approaches are viable management strategies for Crohn’s patients who require a temporary ileostomy
New research identifies a direct functional link between creeping fat and muscle
Retrospective analysis looks at data from more than 5000 patients across 40 years
The Integrated Program aligns IBD care and research across Cleveland Clinic locations
Diet has a profound impact on how the intestine functions