A cost-effective alternative to enoxaparin?
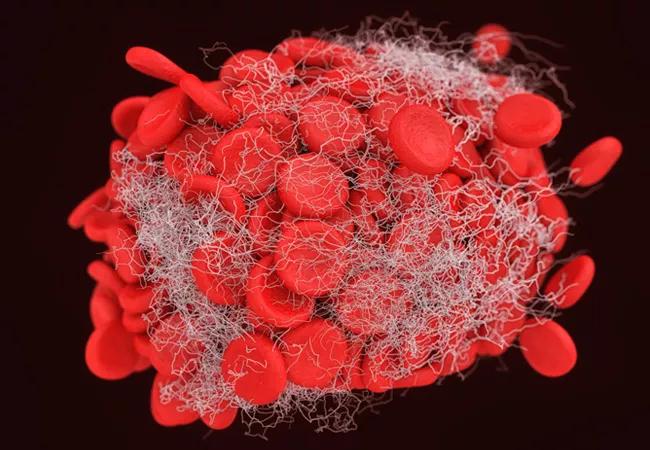
Venous thromboembolism (VTE) extended prophylaxis with low-dose aspirin after inflammatory bowel disease (IBD) surgery is a safe and cost-effective strategy compared with enoxaparin or no prophylaxis, according to a Cleveland Clinic study recently presented at Digestive Disease Week 2021.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Some have challenged the existing guidelines that recommend enoxaparin as a post-discharge medication regimen due to its high cost and the low absolute occurrence of VTE after IBD surgery,” says Stefan Holubar, MD, MS, Inflammatory Bowel Disease Surgery Section Chief and Director of Research in the Department of Colorectal Surgery at Cleveland Clinic’s Digestive Disease & Surgery Institute. “We wanted to discover whether low-dose aspirin could do the job instead.”
Patients with IBD are at higher risk of VTE than the general population and at even greater risk in the postoperative period, depending upon factors including patient age, steroid use, bleeding disorders, type of surgery, postoperative transfusion, pelvic and enterocutaneous fistula surgery, history of hypertension, length of operation and preoperative hospitalization.
The team of Cleveland Clinic researchers and clinicians used primary literature to establish thresholds for post-discharge VTE risk (1.1%) and the efficacy of aspirin and enoxaparin for preventing VTE, bleeding risk and post-VTE sequelae. Then, they developed a decision analysis model that compared outcomes and costs of a reference case patient undergoing IBD surgery. The first round of modeling compared low-dose aspirin to enoxaparin. If low-dose aspirin was more cost effective, a second round of modeling compared aspirin to no prophylaxis. The team analyzed the data from both a healthcare sector perspective and patient perspective.
Enoxaparin showed an unfavorable incremental cost-effectiveness ratio (ICER) of over $900,000 per quality-adjusted life year (QALY) when compared with low-dose aspirin. A 10,000-simulation Monte Carlo probabilistic sensitivity analysis supported this result over 75% of the time.
Advertisement
Low-dose aspirin demonstrated a favorable ICER of just $106,000 per QALY when compared with no extended prophylaxis regimen. Total cost per patient for low-dose aspirin prophylaxis strategies was $54, versus $708 for enoxaparin. From a patient perspective, the cost of a bottle of aspirin is just a few dollars, while the out-of-pocket costs of enoxaparin are one to two orders of magnitude higher, even with insurance.
“We are always concerned with optimal recovery and VTE prevention after surgery, especially for our IBD patients who tend to require multiple surgeries during their lifetimes,” says Dr. Holubar. Cleveland Clinic’s Enhanced Recovery After Surgery (ERAS) protocols are helping speed IBD patients’ healing. Long-acting nerve blocks and non-opioid pain medications minimize patients’ pain from incision through recovery. Patients are encouraged to get out of bed sooner after surgery, accelerating their return to full function and helping prevent postsurgical complications such as VTE. Cost effectiveness is one among many lenses through which Cleveland Clinic research teams are examining optimal recovery strategies.
“Overall, our simulation showed that low-dose aspirin wins in terms of cost and safety when compared with enoxaparin, the current standard, or with no prophylaxis, for our patients undergoing IBD surgery,” says Dr. Holubar. “Our next step is to look at efficacy in these patients, and see if this becomes an attractive, alternative strategy.”
Dr. Holubar is the principal investigator for an ongoing national multicenter collaborative study, funded jointly by the American Society of Colon & Rectal Surgeons and the Crohn’s and Colitis Foundation, which will investigate the topic for the next several years.
Advertisement
Advertisement

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years

Surgical intervention linked to increased lifespan and reduced complications