Advancing our knowledge of risk factors
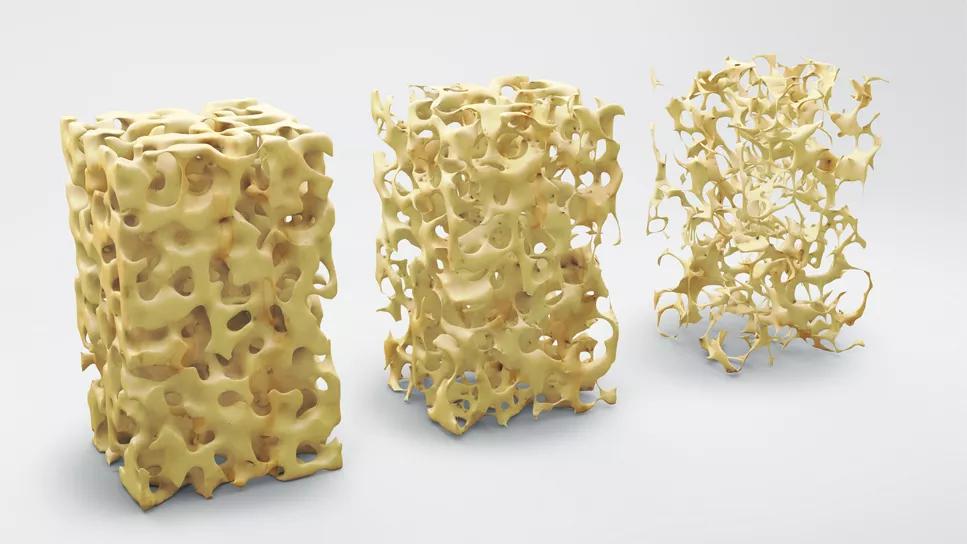
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/fb8c70ce-4f9d-4723-b0a1-d5954c9911c5/bone-structure-osteoporosis-667380856)
Osteoporosis
By Adil Vural, MD, and Sarah F. Keller, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lung transplantation (LT) is a well-established therapeutic option for patients with end-stage pulmonary disease. Patients with end-stage pulmonary disease awaiting LT are more likely to have osteoporosis and fragility fractures than the general population. The prevalence of osteoporosis among these patients is anywhere from 30% to 60%, and vertebral fractures have been detected in 29% of patients with chronic obstructive pulmonary disease and in 25% of patients with cystic fibrosis (CF) awaiting LT.
A number of additional factors increase the risk of bone density loss following LT. Because LT candidates have a high risk of osteoporosis and metabolic bone disease — a risk that increases post-transplant — patients with end-stage pulmonary disease awaiting transplant should be evaluated and treated prior to transplantation. As rheumatologists, we play a critical role in the evaluation and optimization of bone health in these patients.
At Cleveland Clinic, all patients who are evaluated for LT undergo a bone density scan and evaluation by an expert in osteoporosis at the Center for Osteoporosis and Metabolic Bone Disease as part of their pretransplant evaluation.
The association between pulmonary disease and decreased bone density is multifactorial. Underlying lung pathology results in chronic hypoxia and hypercapnia. In CF, additional contributing factors include malabsorption, pancreatic insufficiency, hypogonadism, failure to attain peak bone mass and vitamin deficiencies. Other factors associated with end-stage pulmonary disease such as low body mass index, sedentary lifestyle in patients on chronic supplemental oxygen, older age, female sex and tobacco use also contribute to low bone density. Medication factors pose additional challenges as patients with lung disease are often prescribed proton-pump inhibitors, glucocorticoids and loop diuretics, all of which are associated with bone density loss.
Advertisement
Bone density loss and fractures are also significant problems post-transplant. Post-transplant factors associated with bone density loss include the use of high-dose glucocorticoids, calcineurin inhibitors and mammalian target of rapamycin inhibitors (mTOR inhibitors); calcium and vitamin D deficiencies; and difficulty or failure to adequately ambulate and rehabilitate following surgery. Furthermore, any episodes of graft rejection increase the overall dose of systemic glucocorticoids and subsequent risk of rapid bone density loss.
Typical immunosuppressive regimens in LT recipients include a combination of high-dose, gradually tapered glucocorticoids, cyclosporine, tacrolimus, mycophenolate mofetil and rarely an mTor inhibitor. Osteoporosis and fragility fractures can occur as an early or late complication following transplantation, however the rate of bone loss, and thus fracture risk, is highest immediately following transplantation among patients receiving high-dose glucocorticoids.
Osteoporotic fractures increase morbidity and frailty and pose a significant risk to the patient’s health and survival post-transplantation. Increased vertebral fracture burden has been associated with reduced mobility and physical function, as well as decreased forced vital capacity and inspiratory time. One study found the incidence of vertebral fractures increased from 19.5% pretransplant to 50.4% post-transplant among LT patients in the first period of follow-up (six to 18 months). Another review cited a fracture rate of 18% to 37% in the first post-transplant year. There is clearly a need to decrease bone density decline and fractures following LT.
Advertisement
In addition to the challenges described above, frailty has been increasingly recognized as a potential threat to the survival of patients with end-stage pulmonary disease as well as to those patients who undergo LT. Frailty is a multifaceted clinical syndrome characterized by diminished physical strength which can lead to impaired overall health and reduced survival. An important dimension of frailty assessment is the identification of sarcopenia, a syndrome characterized by decreased muscle mass and progressive decline in physical function that has been associated with fragility fractures, especially in elderly men. While there are several methods of measuring sarcopenia, a novel method involves measuring pectoralis muscle area by computed tomography scan of chest. While sarcopenia and osteoporosis has been examined, in order to better understand the relationship, pathophysiology and mechanisms of sarcopenia and the associated increase risk of fragility fracture, additional research is urgently required which could shed light on potential interventions to improve clinical outcomes.
We are working with an interdisciplinary group to rigorously examine the risk factors for osteoporosis and fragility fractures among LT recipients at Cleveland Clinic. Cleveland Clinic is an international center of excellence for LT and performs a large number of them annually, nearly 2,000 in the twenty-first century. Our objective is to further elucidate the risk factors for osteoporosis, fragility fractures and frailty by analyzing clinical and demographic characteristics, glucocorticoid and other medication use, biochemical and laboratory data, and bone density scans in this large patient population using our unique experience and patient database.
Advertisement
We are working on this multidisciplinary project with co-investigators Abby Abelson, MD, Chair of the Department of Rheumatic and Immunologic Diseases, Chad Deal, MD, Head of the Center for Osteoporosis and Metabolic Bone Disease, Marie Budev, DO, Medical Director of the Lung and Heart Lung Transplant Program, and Xiaojuan Li, PhD, Director of the Program for Advanced Musculoskeletal Imaging. By gaining an enhanced understanding of the risk factors associated with osteoporosis and fragility among patients undergoing LT, developing optimized strategies to prevent bone loss and post-transplant fractures, and creating an improved fracture prediction model for this unique population, we hope to decrease the significant disease burden posed by osteoporosis and metabolic bone among these patients.
Dr. Vural is a resident in the Department of Internal Medicine. Dr. Keller is staff in the Department of Rheumatologic and Immunologic Diseases.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program