Older recipients, multi-organ transplant and coronary artery disease
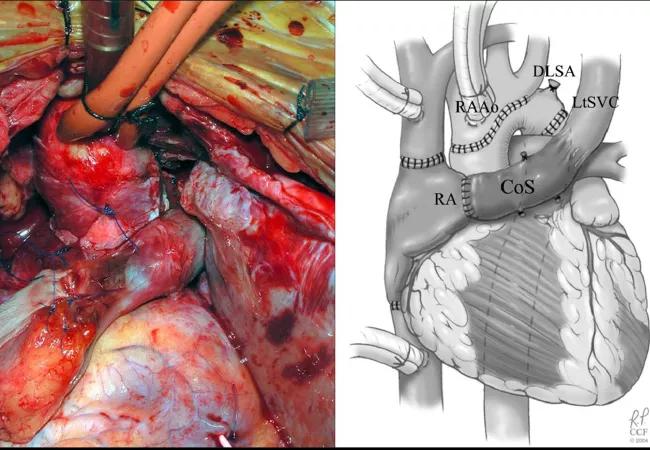
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/16ad9792-4722-4f0f-8d8f-0993cb5145e6/17-PUL-3378-Budev-Hero-Image-650x450pxl_jpg)
17-PUL-3378-Budev-Hero-Image-650x450pxl
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Lung transplantation (LT) has evolved to represent the therapy of choice for a growing number of patients with end-stage lung diseases. In selected patients, LT may significantly prolong survival and improve quality of life. Careful candidate selection is an important part of the effort to increase the likelihood of successful outcomes.
The most recent edition of International Society for Heart and Lung Transplant (ISHLT) Guidelines for the Selection of Lung Transplant Candidates is an excellent guide to help physicians identify patients who are most likely to benefit from LT. However, transplant centers are now being faced with unconventional candidates, and the ISHLT guidelines are limited regarding management of these higher-risk patients who may be older than 65, need multi-organ transplant or have concomitant coronary artery disease (CAD).
Cleveland Clinic’s Lung and Heart-Lung Transplant Program has gained significant expertise in the management and successful transplantation of recipients who are older than 65, have concomitant CAD or may need liver-lung or heart-lung transplantation. Here we share some recent experiences with these nonconventional transplant recipient cohorts.
As life expectancy increases, the proportion of the population over the age of 65 is also growing. As a result, the number of potential LT candidates over the age of 65 is increasing, yet many transplant centers in the U.S. set the cutoff age at 65. Published data regarding outcomes among older LT recipients have been conflicting, precluding firm recommendations. At this time, the decision to transplant candidates older than the arbitrary cutoff age of 65 is center specific.
Advertisement
Cleveland Clinic’s Lung Transplant Program has amassed a significant amount of experience in transplanting candidates over the age of 65 and does not view advanced age alone as a contraindication to transplantation. Our current philosophy is that the numerical value assigned to a person’s age provides an incomplete assessment of the patient’s overall status and suitability for transplant.
Utilizing a multidimensional assessment of a patient’s neurocognitive status, frailty, medical comorbidities and social support, we try to create a composite evaluation that provides more meaningful information than the patient’s chronological age alone. In general, patients of advanced age must be free of any other nonpulmonary complications, and be physically, nutritionally and cognitively capable of undergoing rigorous surgery and postsurgical rehabilitation.
Since our program’s inception in 1990, we have performed 274 LTs in recipients older than 65, including several patients over the age of 75. We have achieved excellent one- and three- year survival in this high risk group.
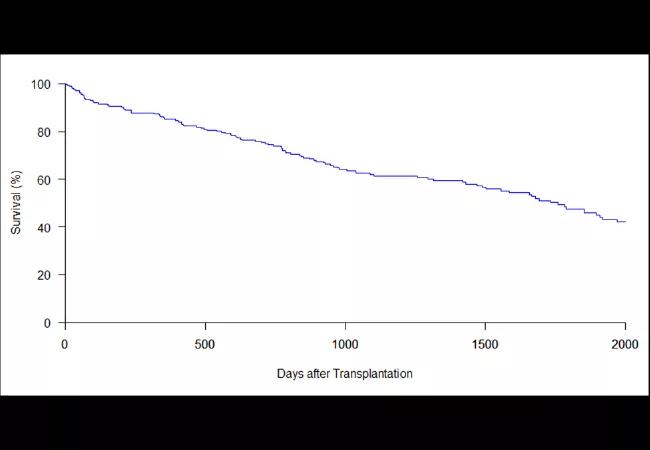
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/e68bc540-68ed-4539-92dc-880b3e8d9e87/17-PUL-3378-Budev-Inset-Chart-650pxl-width_jpg)
Survival curve for patients over 65 years of age (N = 274).
The 2014 ISHLT candidate selection consensus document cites CAD as a relative contraindication. Research from Sudish Murthy, MD, PhD, Section Head of Thoracic Surgery, and colleagues from Cleveland Clinic’s surgical transplant team, however, found that LT recipients who were found to have CAD that could be adequately addressed with either percutaneous coronary intervention or coronary artery bypass grafting (CABG) performed prior to, or concurrent with LT, do not have poorer outcomes. These findings demonstrate that the potential risks posed by the presence of CAD can be mitigated by effective interventions. They highlight the need for an experienced team of interventional cardiologists as well as transplant surgeons skilled in managing the technical complexities of performing LT in patients with prior or concurrent CABG. With this level of experience and expertise at Cleveland Clinic, we have been able to offer transplantation to patients that other centers deemed unsuitable.
Advertisement
Currently, Cleveland Clinic is one of only a few transplant centers in the U.S. to offer heart-lung transplantation (HLT). The leading indication for HLT is adult congenital heart disease, which accounts for almost 35 percent of all of HLT worldwide.
Gosta Pettersson, MD, PhD, Vice Chairman of the Department of Thoracic and Cardiovascular Surgery, and colleagues reported Cleveland Clinic’s experience with 34 HLT procedures performed from 1992-2014. Congenital heart disease was the indication for HLT in approximately 50 percent of cases, and idiopathic pulmonary arterial hypertension accounted for an additional 25 percent of cases. Fifteen percent of the patients who underwent HLT required extracorporeal support (ECMO) as a bridge to transplant Overall survival for the entire group at one, five, 10 and 15 years was 82, 62, 54 and 54 percent, respectively.
Cleveland Clinic is also one of a limited number of centers offering combined liver-lung transplantation (LLT) as a therapeutic option for selected patients with coexisting cirrhotic liver and end-stage lung disease. The main indications for LLT are cystic fibrosis and alpha 1-proteinase inhibitor deficiency, diseases that are prone to both pulmonary and hepatic complications in which the impairment of the liver may jeopardize LT outcomes if performed separately.
Jamak Modaresi Esfeh, MD, staff gastroenterologist, and colleagues recently presented Cleveland Clinic’s experience with five LLT transplants performed between 2000 and 2015. They found that one-year survival for these five combined organ transplant recipients was significantly better than the survival of patients with advanced lung disease and cirrhosis with portal hypertension who underwent LT alone (80 vs. 33 percent, P > 0.001). Thus, for select patients with advanced lung and liver disease, combined transplantation affords an opportunity for extended survival.
Advertisement
Cleveland Clinic’s position as a multispecialty, tertiary care center allows us to perform LT, HLT and LLT on complex, challenging patients. Further, emerging technologies such as ex vivo perfusion and our research on alternative lung allocation models are helping us bring more transplants to more patients. In 2016, we performed 113 LTs and three LLTs. Since our program began in 1990, our long-term survival rates have remained above the national average. As we continue to push the boundaries of LT, we remain centered upon our tripartite mission of better care of the sick, investigation of their problems and further education of those who serve.
Feature image: HLT in a patient with congenital heart disease and Eisenmenger’s syndrome.
Dr. Budev is Medical Director for Lung Transplantation and holds the Macon and Joan Brock Endowed Chair for Lung Transplantation.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program