Patient with intermittent pain and swelling in knee initially appears to have juvenile idiopathic arthritis
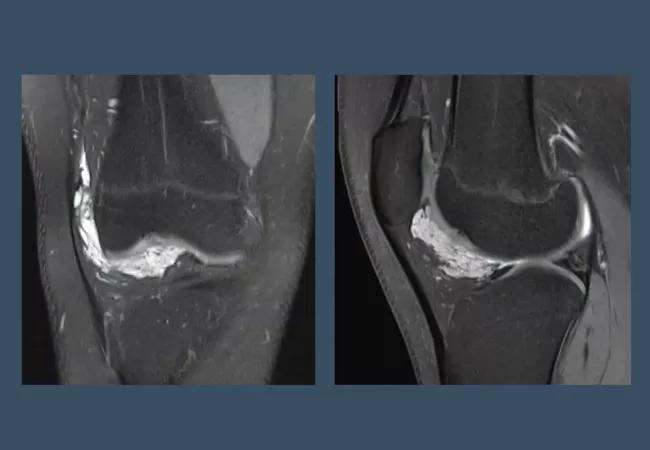
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/ce62a2c6-955f-4ad0-b917-362a7cff14a4/21-RHE-2528508-Arthritis-in-children-Not-just-JIA-CQD_650x450_jpg)
21-RHE-2528508-Arthritis-in-children-Not-just-JIA-CQD_650x450
A 15-year-old male presented with right knee pain and swelling that had been intermittent for ten years.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Upon exam, juvenile idiopathic arthritis (JIA) appeared to be a preliminary diagnosis, although his symptoms were not emblematic of chronic arthritis. The swelling was episodic, occurring only every few months, and typically only lasting less than a week. After that, his knee felt completely normal.
An ultrasound confirmed arthritis in his right knee, but he had no fever or other positive findings for JIA. An X-ray and lab studies, which included: a complete blood count, inflammatory marker test, gonorrhea culture, Lyme disease, rheumatoid factor, cyclic citrullinated peptide antibodies and HLA-B27 tests were all normal. Additionally, the duration of pain and swelling did not support an infectious cause, and he was otherwise healthy without systemic rheumatologic conditions.
Joint aspiration was completed in clinic, allowing the team to retrieve serosanguinous fluid from the joint and inject a steroid.
The patient returned six months later with another episode of pain and swelling in his right knee. This time, the bedside ultrasound revealed an increase in Doppler signal within the Hoffa fat pad, which is not a typical site for synovitis JIA.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/BKWDP1eyHE8?feature=oembed)
Arthritis in Children: Not Just JIA
The team proceeded with an MRI, which revealed a 4 cm mass within the Hoffa’s fat pad. The mass was multilocular with hyperintensity, consistent with synovial hemangioma, a rare benign tumor. He was referred to the Department of Orthopaedics, where the team led an arthroscopic excision of the mass and synovectomy.
The diagnosis, confirmed on histopathology, explained the off-and-on knee swelling was caused by episodic intraarticular bleeding and hemosiderotic synovitis.
Advertisement
In this case, JIA was a diagnosis of exclusion. When it comes to arthritis in children, maintain a broad differential of potential etiologies.
Advertisement
Advertisement
Findings hold lessons for future pandemics
One pediatric urologist’s quest to improve the status quo
Overcoming barriers to implementing clinical trials
Interim results of RUBY study also indicate improved physical function and quality of life
Innovative hardware and AI algorithms aim to detect cardiovascular decline sooner
The benefits of this emerging surgical technology
Integrated care model reduces length of stay, improves outpatient pain management
A closer look at the impact on procedures and patient outcomes