Regular surveillance necessary to identify safety signals
An analysis of real-world evidence from large registry-based data confirmed the increased incidence of cardiovascular events in chronic lymphocytic leukemia (CLL) patients treated with ibrutinib, and showed this treatment is associated with higher incidence of major bleeding events than was found in initial studies. A new study at Cleveland Clinic published in the Journal of American College of CardioOncology found a significant increase in major bleeding and a borderline increase in stroke risk, which had not been previously reported.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
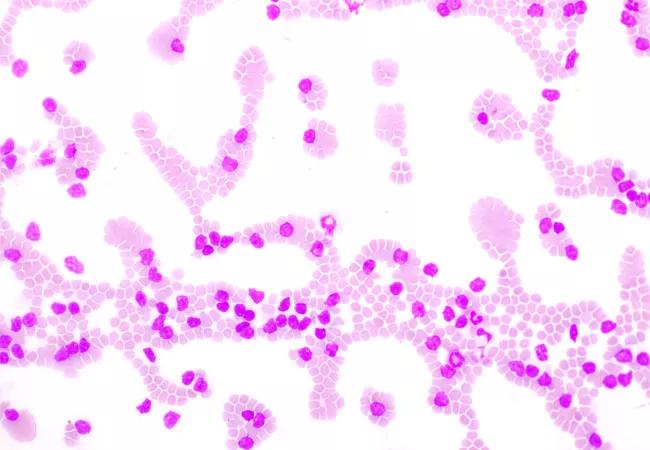
Ibrutinib is a first-in-class Burton’s tyrosine kinase (BTK) inhibitor. Early Ibrutinib trials recognized an association with specific adverse events such as bleeding and atrial fibrillation in younger patients treated for CLL. However, most clinical trials have enrolled patient populations of lower median age than the CLL population overall, which has limited information about these risks specifically in older patients with CLL.
Using the Surveillance, Epidemiology and End Results Program (SEER) data linked with Medicare claims, the research team identified patients diagnosed with CLL between 2007-2015, with 4,958 meeting inclusion criteria. The median age of the study population was 78 years. Sixty-one percent of patients had not yet received treatment for CLL, 32.7% were treated with agents other than ibrutinib, while 6% were treated with ibrutinib. In evaluating SEER data, researchers found that among patients treated with ibrutinib, the risk of major bleeding and stroke was higher than previously found in clinical trials.
Patients treated with ibrutinib had a 4.9-fold increased risk of bleeding (HR: 4.92; 95% CI: 3.36-7.01) and a 7.5-fold increased risk of major bleeding (HR: 7.49; 95% CI; 4.32-12.99) compared to those on other therapies. Patients treated with ibrutinib also had an increased risk of atrial fibrillation (HR: 3.65; 95% CI: 2.5205.49) compared to patients treated with other therapies.
“One of the challenges of clinical trials in general is that it’s not always easy to enroll patients of more advanced age, as they tend to have more comorbidities, so you tend to see adverse events are a bit more pronounced in registry data than in a clinical trial,” explains Paolo Caimi, MD, study co-author and a hematologist-oncologist with Cleveland Clinic. “Ibrutinib has been shown to control disease better than chemotherapy and is very safe, but these study data show what practicing physicians already know, which is to monitor patients closely for new or more pronounced adverse events when prescribing a new drug, particularly in patients who are older and may be more frail.”
Advertisement
The study findings highlight the importance of early and frequent surveillance, particularly in older patients being treated for CLL. “Having access to a specialist who can help manage adverse events like atrial fibrillation or evaluate a patient’s cardiac risk is important when a patient is starting on a new therapy,” says Dr. Caimi. “If a patient is at risk of cardiac issues, having a cardio-oncologist readily available to support them is very helpful.”
Informing patients helps them to monitor for symptoms. “Patients should also be made aware of the risks, so they can proactively consult if they have symptoms suggestive or arrhythmia, and awareness of a higher risk of more severe bleeding can prompt them to seek care early in case of a fall or another accident. Working in partnership with patients can help to reduce adverse events and their severity.”
Advertisement
Advertisement

Discussing research into improving CAR T-cell therapy efficacy

Blinatumomab plus chemotherapy improves overall survival and relapse-free survival over chemotherapy alone

Large trial shows efficacy and lower incidences of heart issues and bleeding events with novel non-covalent BTK inhibitor

Single-cell next-gen sequencing showing promise to improve sensitivity of MRD testing

Scenarios where experience-based management nuance can matter most

Aim is for use with clinician oversight to make screening safer and more efficient

Study shows significantly reduced risk of mortality and disease complications in patients receiving GLP-1 agonists

Tasked-based therapy improves social connection and quality of life