New review makes the case for earlier pediatric enrollment and other changes
Despite the growing number of disease-modifying therapies (DMTs) for multiple sclerosis (MS), only one is approved for use in children. This is a challenge for physicians like Aaron Abrams, MD, and Mary Rensel, MD, who see increasing evidence that early, targeted treatment of pediatric-onset MS (POMS) can help offset long-term disability. Dr. Abrams is a pediatric MS and neuroimmunology specialist in the Center for Pediatric Neurosciences and Dr. Rensel is an MS expert in the Mellen Center for Multiple Sclerosis, both within Cleveland Clinic’s Neurological Institute.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In a recent narrative review in touchReviews in Neurology (2022;18[1]:42-48) they wrote with Cleveland Clinic colleagues, Drs. Abrams and Rensel conclude that the tradition of completing MS clinical trials with adult subjects before enrolling any pediatric patients may not be in the best interest of young patients with MS. Including pediatric patients in adult trials should be a research priority, the authors contend, noting that support is increasing among MS specialists for starting DMT treatment as early as possible in POMS.
The review points out that most information on DMT in pediatric MS patients comes from two retrospective analyses published in 2018 and 2020, each of which used clinical data collected since 2011 from a network of pediatric MS centers. The analyses found that early initiation of highly effective DMT had favorable outcomes compared with use of first-generation injectable therapies, with safety profiles similar to those seen in adults.
Since 2019, at least four new phase 3 investigations have been initiated to evaluate the safety and efficacy of DMTs in pediatric patients with MS. “We are optimistic that the results of these trials may provide further support for starting treatment with DMTs in pediatric patients, and that positive results could facilitate insurance coverage and increase physician comfort with prescribing newer DMTs to pediatric patients,” says Dr. Abrams.
He notes that Cleveland Clinic will serve as a participating site in one of the four phase 3 investigations, which will compare fingolimod and ocrelizumab. Fingolimod, an oral medication, is currently the only DMT approved by the FDA for use in pediatric patients. Ocrelizumab is an infusion therapy that has proven to be highly effective in adult MS and has also been studied in early-phase POMS research trials in which the Mellen Center has been a participating site.
Advertisement
The other phase 3 studies include comparisons of dimethyl fumarate with peginterferon beta-1a, ofatumumab and siponimod with fingolimod, and peginterferon beta-1a with interferon beta-1a.
According to Dr. Rensel, both the United States and Europe recently mandated a good-faith effort by the pharmaceutical industry for completion of POMS treatment trials. “However,” she says, “completion of such trials is often difficult because POMS is relatively rare and patient recruitment is a challenge due to distance, school and work schedules.” On the rarity issue, she notes that POMS accounts for an estimated 5% to 10% of patients with MS, although these numbers are thought to be an underestimate.
The TERIKIDS trial, which evaluated teriflunomide for treatment of POMS, involved 57 centers across 22 countries, enrolling 166 patients over 5 years, while its adult counterpart trial enrolled 1,088 patients over 4 years at 127 centers in 21 countries. Despite the TERIKIDS trial achieving positive trends similar to those observed in the adult trial, the primary outcome did not reach statistical significance. It was thought the small sample size left the study underpowered. Even so, the European Union approved teriflunomide for treatment of POMS, but the FDA has not.
“If we don’t apply new strategies to our trials,” Dr. Abrams observes, “underpowered studies will continue to hinder FDA approvals.”
In 2019, the International Pediatric Multiple Sclerosis Study Group issued guidelines for the design, recruitment and completion of POMS clinical trials. Among their recommendations:
Advertisement
“The conventional wisdom that adult trials must be completed before pediatric patients can be included creates significant delays in getting FDA approval for pediatric use,” says Dr. Abrams, noting that fingolimod was approved for adults in 2010, but 8 years passed before it was approved for pediatric patients. “It’s time to prioritize including pediatric patients in adult trials.”
“At Cleveland Clinic,” says Dr. Abrams, “we’re actively working to achieve one of the goals we laid out in touchReviews in Neurology — to develop research trials that focus on new therapies specifically in the pediatric MS population.”
Dr. Abrams and Dr. Rensel emphasize that with a pediatric demyelinating disease like POMS, an outcome of better neurologic function down the line depends on early intervention with high-efficacy medication.
“Any patient or parent concerned about possible neuroimmunologic disease needs to know how important it is to seek out a specialist for a full evaluation,” he says. “Only then can we provide the best information and therapy available.”
Advertisement
Advertisement

Mixed results from phase 2 CALLIPER trial of novel dual-action compound

A co-author of the new recommendations shares the updates you need to know

Rebound risk is shaped by patient characteristics and mechanism of action of current DMT

First-of-kind prediction model demonstrates high consistency across internal and external validation

Real-world study also finds no significant rise in ocrelizumab-related risk with advanced age

Machine learning study associates discrete neuropsychological testing profiles with neurodegeneration

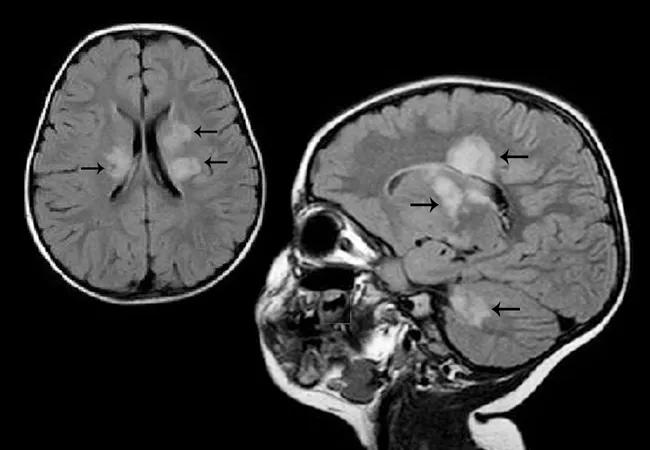
This MRI marker of inflammation can help differentiate MS from mimics early in the disease

Focuses include real-world research, expanding access and more