About this condition and the effectiveness of clomiphene
In this Q&A with Consult QD, endocrinologist Guy Mulligan, MD, in Cleveland Clinic’s Department of Endocrinology, Diabetes and Metabolism, provides an update on the use of clomiphene in male hypogonadotropic hypogonadism.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
What are the main causes of hypogonadotropic hypogonadism in men?
A: Hypogonadotropic hypogonadism, also known as secondary hypogonadism, is caused by disfunction of the pituitary gland, which leads to insufficient production of testosterone in men. For distinction, primary hypogonadism is caused by disfunction of the testes.
Two types of pituitary disfunction can cause hypogonadotropic hypogonadism: one is damage to the gland itself, for example, due to a mass, inflammation or radiation therapy to the head or neck, and the other is suppression of pituitary gland hormones. Pituitary gland hormones may be suppressed as a consequence of steroid use, high levels of prolactin—another pituitary hormone, or an excess of estrogen due to obesity/insulin resistance.
What percent of men are affected by this condition?
A: It is hard to give an exact percentage, but the incidence rate is probably very similar to the current rate of obesity in men. Most men are initially diagnosed in the age range of 35 – 50 years old.
What is the standard treatment for male hypogonadotropic hypogonadism?
A: Men are given different transdermal preparations, such as testosterone-containing patches or gels, or intramuscular injections of testosterone. Intramuscular injections are probably the most reliable approach because they assure that the patients are getting the full dose of the medicine and that dose can be easily adjusted. These treatments aim to relieve fatigue, improve muscle strength, libido and erectile function, as well as relieve anxiety, depression and irritability.
Advertisement
What is the main mechanism of action of clomiphene in male hypogonadotropic hypogonadism?
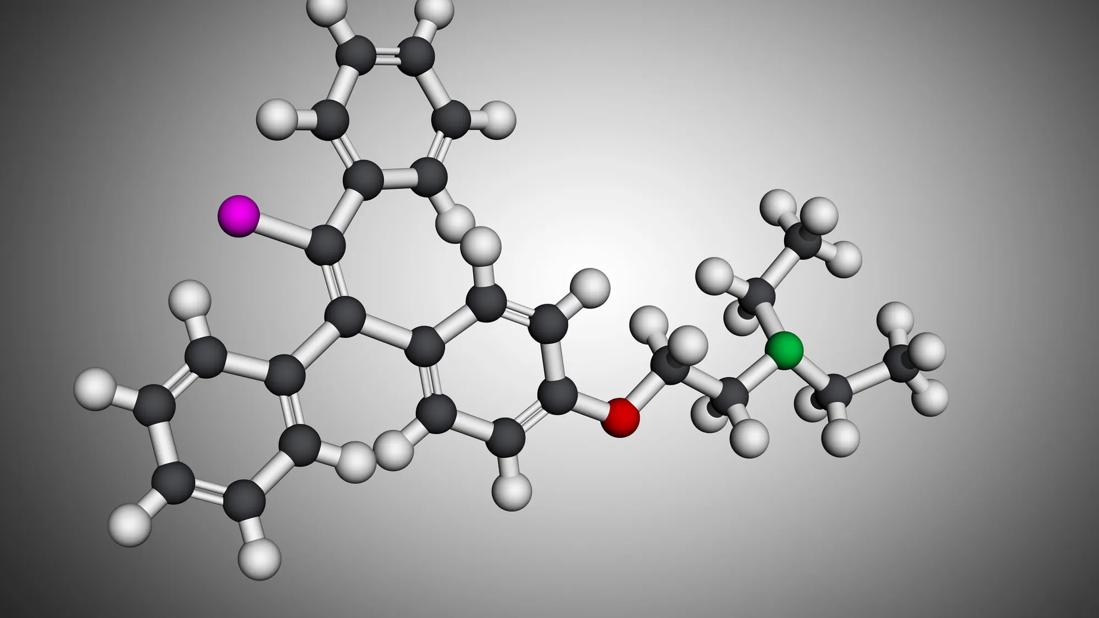
A: Clomiphene is a selective estrogen receptor modulator (SERM). It works by interacting with the estrogen receptor on the pituitary gland. Clomiphene binds to this receptor and blocks the effects of estrogen on the pituitary gland.
In normal physiology, the gonadotropins are released from the pituitary and stimulate the testes to produce testosterone. A small amount of testosterone is then converted into estrogen which becomes the “off” signal for the pituitary to stop producing testosterone. In obese and insulin resistant patients, adipose tissue also produces estrogen which signals the pituitary gland to stop producing hormones. Clomiphene helps by blocking that estrogen feedback and reducing the “off” signal to the pituitary, so that it can further stimulate the testes to produce testosterone. This way, clomiphene helps interrupt the pathway that leads to hypogonadotropic hypogonadism.
Is clomiphene currently approved by the FDA for the treatment of male hypogonadotropic hypogonadism?
A: No, use of clomiphene in male hypogonadotropic hypogonadism is an off-label use of the medicine.
How much clinical evidence supports the use of clomiphene in male hypogonadotropic hypogonadism?
A: Clomiphene’s primary use is for fertility treatment in women. But because the hormone pathways are similar in men and women, it has also been used on an off-label basis for infertility in men. There is now an increasing number of studies from different groups around the country showing that clomiphene, given in doses ranging from 25 mg every other day up to 50 mg every day, improves testosterone levels in patients with obesity and insulin resistance.
Advertisement
How effective is clomiphene in helping men with hypogonadotropic hypogonadism achieve symptom relief?
A: Overall, the studies report variable efficacy of clomiphene in reaching symptom relief. In my own clinical practice, I have noticed that a number of patients get a very good response in terms of testosterone level but may feel that their symptoms are not well relieved. However, clomiphene does have several advantages: (1) it is given as a tablet so it is easier to administer than injections, (2) due to its off-label use, it is cheaper than standard treatments for hypogonadotropic hypogonadism, (3) it has a beneficial effect on male fertility, because the testes are more effectively stimulated with clomiphene, (4) one study showed a reduced chance of patients developing polycythemia with clomiphene in comparison to standard testosterone replacement treatment.
What is your clinical experience with clomiphene in male hypogonadotropic hypogonadism?
A: I usually suggest this treatment approach for the obese, insulin-resistance, men, which is the most common group of patients I see. Most of the time, my patients achieve a good biochemical response to clomiphene and produce higher amounts of testosterone.
In terms of symptom relief, approximately two thirds of men feel better, while about a third don’t feel like they are getting the benefit. There are two types of side-effects that are unique to clomiphene, ophthalmologic and psychiatric, which I have seen on occasion. If patients complain of ophthalmologic issues, such as “floaters” of blurry vision, we have to stop treatment. Sometimes clomiphene can exacerbate psychiatric conditions; for example, it can make depressive symptoms worse. While these side effects are very rare, they are possible.
Advertisement
Advertisement

Pheochromocytoma case underscores the value in considering atypical presentations

Advocacy group underscores need for multidisciplinary expertise

A reconcilable divorce

A review of the latest evidence about purported side effects

High-volume surgery center can make a difference

Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D

Patients spent less time in the hospital and no tumors were missed

A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications