A comprehensive approach to genitourinary syndrome of menopause
A 46-year-old patient presented to our specialty women’s health clinic with vaginal bleeding. Previously, this patient was treated at our facility for early-stage breast cancer. As part of her treatment, she had a hysterectomy, oophorectomy and was on a long-term adjuvant course of aromatase inhibitors (AIs).
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
The patient was very concerned that the etiology of the bleeding was cancerous.
On exam, we determined that a urethral caruncle—a large friable red mass—was the source of the bleeding, which was the result of marked hormonal deficiency of the lower genitourinary system.
Treatment included a temporary suspension of the aromatase therapy and a course of topical vaginal estrogen to resolve the urethral caruncle. Following symptom resolution, adjunctive therapy resumed.
This is a dramatic example of a complication of AI therapy in women with estrogen receptor-positive breast cancer. AIs inhibit the enzyme aromatase, which promotes the conversion of androgen into estrogen, reducing breast cancer recurrence and improving overall survival.
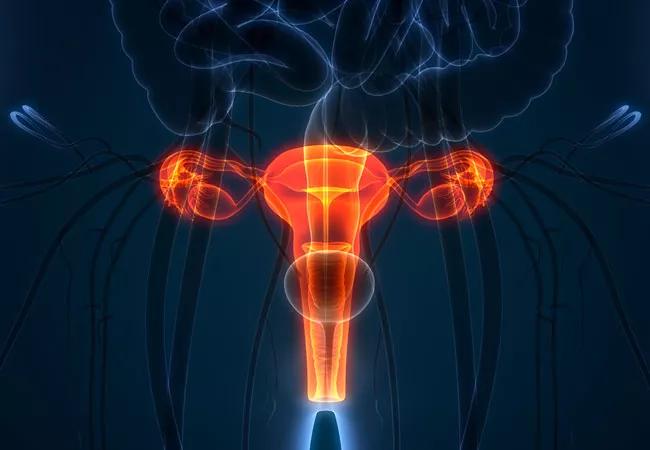
However, systemic loss of estrogen results in changes to the genital structures and vaginal mucosa, including the following:
These symptoms are known as genitourinary syndrome of menopause (GSM), and can have a significant impact on a patient’s quality of life.
“It’s not just a minor lifestyle problem,” says Holly L. Thacker, MD, Professor and Director of Cleveland Clinic Center for Specialized Women’s Health. “There’s a lot of significant known risk of untreated atrophy: bleeding, pain, sexual dysfunction, destroyed relationships, recurrent bladder infections that can even lead to urosepsis.”
Advertisement
GSM is the topic of a clinical review recently published by a team of Cleveland Clinic oncologists and a women’s health specialist in the Journal of Oncology Practice.
“This topic is not always addressed with breast cancer survivors on endocrine therapy, and is an important topic for quality of life and safety in patients,” states Tamara Sussman, MD, lead author on the study. “Hopefully, our review will help guide this important conversation and management of GSM of menopause in this patient population. Most importantly, we hope that this article will help oncologists to have meaningful and helpful conversations about GSM with their patients on endocrine therapy.”
Nonhormonal treatments such as vaginal gels, moisturizers and lubricants, can temporarily relieve symptoms of atrophy by increasing moisture. They are considered safest for women with hormone-related breast cancer, but do not change the underlying disorder. Nevertheless, when used regularly, vaginal moisturizers can alleviate symptoms of vaginal dryness and itching. Vaginal lubricants can be added to reduce friction during intercourse.
Vaginal estrogen therapies—in the form of estradiol-releasing intravaginal tablets, low-dose estrogen vaginal inserts, estrogen-based vaginal creams and estradiol-releasing vaginal rings—improve GSM symptoms with varying levels of systemic absorption. The newest vaginal estradiol currently on the market is Imvexxy®, a vaginal insert that comes in 4-µg and 10-µg doses in bio-adhesive coconut oil.
Advertisement
Non-estrogen therapy with precursor vaginal DHEA—as in Intrarosa®—can be offered in women declining even local, very low dose estrogen therapy and/or in women for whom the local estrogen therapy is not enough. Vaginal DHEA is aromatized to estrogen and testosterone in intracellular vaginal tissue.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors