Common motility issues, indications for testing, and when to refer your patient

By the time patients see Ben Freiberg, MD, a pediatric gastroenterologist at Cleveland Clinic Children’s, they have likely already failed primary interventions for symptoms related to gastrointestinal (GI) dysfunction. His goal is to enhance medical management, measure their GI motility, and evaluate their candidacy for surgical intervention.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
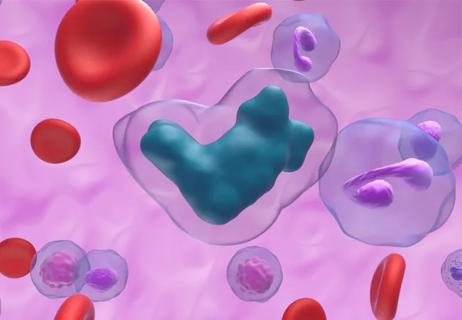
GI motility disorders are classified as the dysregulation of movement in the digestive system and of the contents within. Dr. Freiberg and his colleagues treat a variety of symptoms related to this dysfunction in children and adolescents.
Constipation is very common among the patients Dr. Freiberg treats. About a quarter-to-half of his patients present with refractory constipation, a symptom related to dysmotility in the colon.
“It’s also not uncommon for us to see esophageal dysphagia as well as nausea and vomiting, raising concerns for gastroparesis, a delayed emptying of the stomach into the small intestine,” he says. Other symptoms seen may include gastroesophageal reflux disease, chest pain, irritable bowel syndrome, dyspepsia, diarrhea and more.
This has made studies that evaluate the function of the esophagus, small intestine and colon particularly important, leading Cleveland Clinic Children’s to offer a variety of different types of manometry studies, including esophageal, antro-duodenal, anorectal and colonic as well as endoluminal functional lumen imaging probe (EndoFLIP™).
Esophageal manometry. A short catheter is placed through the nose into the patient’s esophagus. Pressure sensors measure esophageal peristalsis and relaxation of the lower esophageal sphincter. This test is used to determine if children with dysphagia have achalasia, esophagogastric junction outflow obstruction, or a disorder of peristalsis.
EndoFLIP. An inflatable balloon with sensors is placed into the esophagus under anesthesia and measures distensibility, providing information on esophageal wall stiffness and the esophagogastric junction. It is used in patients with achalasia and eosinophilic esophagitis.
Advertisement
Antro-duodenal manometry.In this procedure, a pressure-sensing catheter is inserted into the patient’s esophagus, through the stomach, and into the small intestine while they are under anesthesia. The patient is monitored over six hours to evaluate the function and intestinal response during fasting, eating and provocative medications (to induce contractions).
Anorectal manometry. Typically, this is the first manometry study done for constipation. A short catheter with pressure sensors and a balloon at the tip is placed through the anus into the rectum. It is used to measure how well the muscles and nerve endings in the rectum and anus are working. It can diagnose patients with Hirschsprung’s disease or dyssynergic defecation.
Colonic manometry. Similar to the antro-duodenal procedure, a pressure-sensing probe is inserted through the anus and into the colon while the patient is under anesthesia. Patients are similarly monitored over six hours to evaluate the function and colonic response to fasting, eating and provocative medications.
Changes in diet and lifestyle, such as toilet training, may prompt constipation or withholding behaviors, explains Dr. Freiberg. For example, the introduction of solid foods or whole milk can lead to harder stool formation and subsequent constipation. Toilet training can also motivate a child’s functional autonomy and desire for control, which may result in patterns of chronic withholding.
Lifestyle modifications to diet, like increased fiber and fluid intake, or other outpatient counseling programs, like Cleveland Clinic Children’s “Poop School” should be considered. But when these aren’t effective, Dr. Freiberg encourages pediatricians to get an early start on medication management.
Advertisement
“Start with a powder-based stool softener mixed in liquid, and if the child isn’t responding well, it may be appropriate to start a stimulant medication. And once you’re at that point, it’s also a good time to involve a GI specialist,” he says.
Dysmotility associated with upper digestive tract dysfunction can be congenital or develop spontaneously later in life, explains Dr. Freiberg. Though diet and/or developmental changes may play a role in dysfunction, it’s important to maintain clinical suspicion for GI dysmotility, provide early intervention as needed, and be prepared to refer to a specialist if that treatment fails.
“By the time the child is evaluated by a GI specialist, we will aim to optimize their regimen if needed and take a closer look at the issue. Are there other medications we can try? Should we begin to consider surgical intervention? That’s really when we start to talk about implementing these studies and determine the next best step,” concludes Dr. Freiberg.
Advertisement
Advertisement

Greater awareness among young patients is needed

Customized interventions for GI disorders are enhancing patient outcomes

Careful risk stratification is key

A three-step plan aimed at strengthening the institute’s infrastructure includes a renewed focus on mentorship

Hard-to-treat GI disorders benefit from multidisciplinary approach
Researchers compared tacrolimus/methotrexate to tacrolimus and reduced-dose methotrexate/mycophenolate

Newer medications pivotal for improving gastrointestinal symptoms in patients with cancer

Beyond recognizing and treating food allergies, GIs also have a responsibility to address common food allergy misconceptions