Long-term safety and efficacy assessed
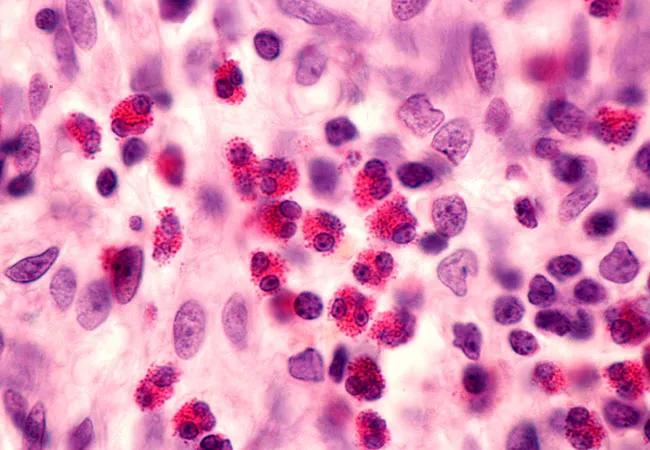
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5ba7543e-063b-45a4-b99a-bb2b9fb20912/650x450-Eosinophil_jpg)
650×450-Eosinophil
By Sumita Khatri, MD
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Severe asthma is a heterogeneous condition in which patients present with different clinical and physiologic characteristics and display differing treatment responses. The addition of biologics to standard-of-care asthma therapy has introduced a more personalized treatment approach for patients with severe asthma, providing a direct benefit in reducing exacerbations and improving other markers of asthma control. However, there are limited data evaluating the long-term safety of these biologics and the durability of the treatment response.
Mepolizumab, an anti-IL-5 humanized monoclonal antibody, is recommended as a step five therapy option for patients with severe eosinophilic asthma (SEA). The efficacy and safety of mepolizumab in patients with SEA has been demonstrated, with strong and consistent exacerbation reductions in four randomized placebo-controlled trials. However, the long-term safety of mepolizumab beyond 12 months has not been reported. The COLUMBA study sought to fill that gap with an open-label, long-term extension in patients who participated in the DREAM study (Dose Ranging Efficacy And Safety With Mepolizumab in Severe Asthma). The primary objective was to describe the safety profile of mepolizumab in patients receiving long-term treatment. The effects of mepolizumab on a range of clinical markers of asthma control were also assessed.
COLUMBA (Open-Label Long Term Extension Safety Study of Mepolizumab in Asthmatic Subjects) was an open-label, multicenter extension study in patients with SEA previously enrolled in DREAM. DREAM was a randomized, double-blind, placebo-controlled trial of mepolizumab in patients with SEA (aged > 12 years). Patients were invited to participate in COLUMBA 12 to 28 months after they completed the DREAM study. In the COLUMBA study, patients received 100 mg of subcutaneous mepolizumab every four weeks plus standard of care until a protocol-defined stopping criterion was met. Safety end points included frequency of adverse events (AEs), serious AEs and AEs of special interest. Efficacy end points included annualized exacerbation rates, changes from baseline in Asthma Control Questionnaire 5 scores and blood eosinophil counts. We also assessed immunogenicity.
Advertisement
The study enrolled 347 patients for an average of 3.5 years. On-treatment AEs were reported in 94 percent of patients, with the most frequent being respiratory tract infection, headache, bronchitis and asthma worsening. Twenty-three percent of patients experienced one or more on-treatment serious AEs; there were six deaths, none of which were assessed as related to mepolizumab. The only on-treatment drug-related AEs reported with an incidence 3 percent or greater were injection-site reactions and headache. Overall, no new safety concerns were identified in this study after long-term exposure.
Patients with 156 weeks or greater enrollment experienced a 56 percent reduction in exacerbations from the off-treatment period between DREAM and COLUMBA. For all patients, at the first post-baseline assessment, the mean Asthma Control Questionnaire 5 score was reduced by 0.47 points, and blood eosinophil counts were reduced by 78 percent, with similar improvements maintained throughout the study. The immunogenicity profile (8 percent anti-drug antibodies) was consistent with previous studies.
This study represents the longest clinical experience to date with an anti–IL-5 monoclonal therapy in patients with severe asthma. The results of this long-term open-label extension with mepolizumab exposure for up to 4.5 years in patients with SEA add to the overall safety profile of mepolizumab in this patient population. This study additionally demonstrates the durability of clinical and pharmacodynamic responses after long-term mepolizumab treatment, with improvements consistent with those reported in previous randomized clinical trials and maintained for up to 4.5 years. Overall, these results support the use of mepolizumab as a long-term treatment choice for patients with SEA.
Advertisement
Dr. Khatri codirects the Asthma Center in the Respiratory Institute.
Advertisement
Advertisement
Takeaways from the most recent annual meeting centered around clinical advances, AI integration and professional development
Recent breakthroughs have brought attention to a previously overlooked condition
A review of treatment options for patients who may not qualify for surgery
Looking at the real-world impact and the future pipeline of targeted therapies
The progressive training program aims to help clinicians improve patient care
New breakthroughs are shaping the future of COPD management and offering hope for challenging cases
Exploring the impact of chronic cough from daily life to innovative medical solutions
How Cleveland Clinic transformed a single ultrasound machine into a cutting-edge, hospital-wide POCUS program