Patients report improved sense of smell and taste
Loss of smell and taste are among the most common symptoms after COVID-19 infection. While a survey published in the International Forum of Allergy & Rhinology indicates that nearly half of those who report olfactory dysfunction regain their sense of smell within a month, the problem can linger.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“I am still seeing patients who had the initial infection in 2020, and for the last three years they have been silently suffering from altered smell and/or taste,” says Christina Shin, MD, a Cleveland Clinic pain management physician.
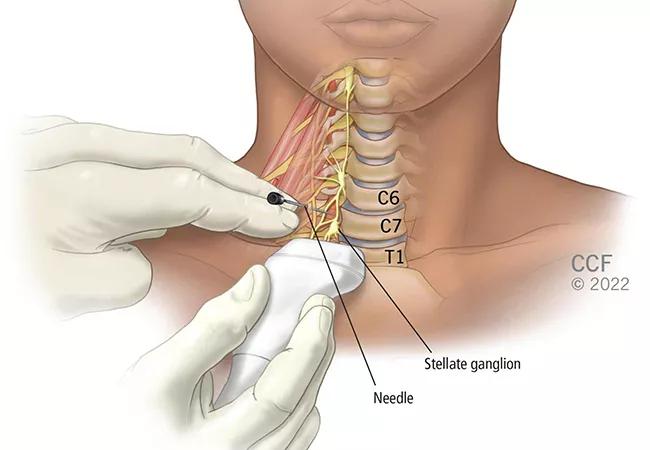
Olfactory and gustatory training is the first-line recommended treatment. But when it fails, patients are increasingly turning to Dr. Shin and other pain management physicians for a novel treatment – stellate ganglion block (SGB).
In the past year, Dr. Shin has administered the stellate ganglion block with ultrasound imaging guidance to approximately 40 patients. Her first patient arrived to the initial consultation with a case series published by Luke Liu, MD, a pain medicine specialist in Anchorage, Alaska, who pioneered the use of SGB to reduce symptoms in patients with long COVID.
“I don’t tout this as a cure,” says Dr. Shin. “In review of my clinical experience caring for patients, I would conservatively estimate that at least 50% of patients achieve at least 50% improvement. Of course, further research is needed.”
One year after her stellate ganglion block, Dr. Shin’s first patient reports a 90% improvement. That has had a tremendous impact on her quality of life, given that for two years food tasted rancid.
“She is back to work, spending time with family and enjoying her social life,” says Dr. Shin. “She is also off anti-depressants.”
Stellate ganglion block targets the sympathetic system, specifically the face and upper extremities. Indications include complex regional pain syndrome of the head and upper limbs, postherpetic neuralgia, hyperhidrosis, chronic post-surgical pain, peripheral vascular disease, and orofacial pain.
Advertisement
It’s unclear how SGB works for patients with loss of smell and taste – or even what causes long COVID – but experts posit several theories.
First, long COVID: One theory is that the virus directly invades tissues in the lungs, nasal mucosa and brain, causing destruction. Another is that the immune system becomes hyperactive in response to the infection, leaving patients in a state of persistent inflammation. A third hypothesis suggests that the sympathetic system is in overdrive, persistently active, leading to fatigue and other long COVID symptoms.
“The fact that the stellate ganglion block is working for some patients tells us that at least for those patients, it may be related to the persistent, overactive sympathetic system,” says Dr. Shin. “So, when we temporarily stop activity at that bundle of nerves and patients get better, perhaps we are interrupting this overactivity and allowing their bodies to reset and get back to a more normal sympathetic balance.”
Another possibility is that the stellate ganglion and the sympathetic system are closely connected to the immune system.
“The thought is that by modulating or blocking the sympathetic system, we somehow regulate the immune system,” says Dr. Shin.
Finally, when the stellate ganglion is blocked, blood flow increases to that side of the body and the brain. That may improve signaling of existing neurons involved in the processing of smell and taste.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/erMPoEr8Bgo?feature=oembed)
Woman Smells for First Time in Two Years With Long COVID
Jijun Xu, MD, PhD, who holds joint appointments in Cleveland Clinic’s Department of Pain Management and the Department of Inflammation and Immunity at Lerner Research Institute, also has administered stellate ganglion blocks. Although SGB is a well-defined treatment in pain management, he stresses that its use for olfactory disorder associated with COVID-19 is still experimental and not effective for all patients. However, he considers it a viable option for some patients.
Advertisement
“When SGB works, it seems to work effectively,” says Dr. Xu. “Considering its low risk profile and potential benefit, SGB is worth trying for these patients as it may significantly help improve a patient’s quality of life. More importantly, some patients lose their ability to smell gas in heating appliances or cooking equipment, which could be dangerous or even life-threatening. To bring their smell back is therefore of the utmost importance.”
Patients may require follow-up treatments similar to SGB use for pain management.
At Cleveland Clinic’s reCOVer Clinic for long COVID patients, Dr. Shin is collaborating with ENT specialists to outline indications and develop a pathway for patients with loss of smell and taste who may benefit from SGB. She currently evaluates patients who have had a confirmed COVID-19 diagnosis and have been diagnosed with COVID-related smell and taste disorder. She also encourages patients to see an ENT specialist first to make sure there isn’t an underlying issue.
“If you have a primary smell and taste disorder from trauma, sinusitis or other conditions, the nerve block may not change that,” says Dr. Shin.
In addition, contraindications for stellate ganglion block include glaucoma, coagulopathy, recent myocardial infarction, severe pulmonary disease, pre-existing counter lateral nerve palsy and cardiac conduction block. Potential risks of the procedure include bleeding and infection, as well as puncture of nearby structures, such as the trachea, esophagus, carotid artery and internal jugular.
Advertisement
“Overall, it’s a safe procedure, and we have found ways to improve the safety over the last several years, especially when it is image-guided, such as with ultrasound,” says Dr. Shin.
Dr. Shin suggests that physicians caring for patients with COVID-related olfactory disorder take the following steps:
“I am cautiously optimistic about this experimental treatment,” says Dr. Shin. “In the right person – someone who doesn’t have contraindications and the benefit outweighs the risk – the stellate ganglion block may be utilized for COVID-related smell and taste disorders.”
Advertisement
Advertisement

Dynamic modeling improves the accuracy of outcome predictions for ICU patients

A review of IDSA and NIH guidelines

Study sheds light on how clinicians addressed their patients’ pain and insomnia during the pandemic

Clinicians who are accustomed to uncertainty can do well by patients

Unique skin changes can occur after infection or vaccine

Will enable patients with long COVID to enroll in national clinical trials

Cleveland Clinic analysis suggests that obtaining care for the virus might reveal a previously undiagnosed condition

Team collaborates to explore effects of genetic mutations to proteins OAS and RNase L