AUA review consolidates and updates two earlier documents into one evidence-based document
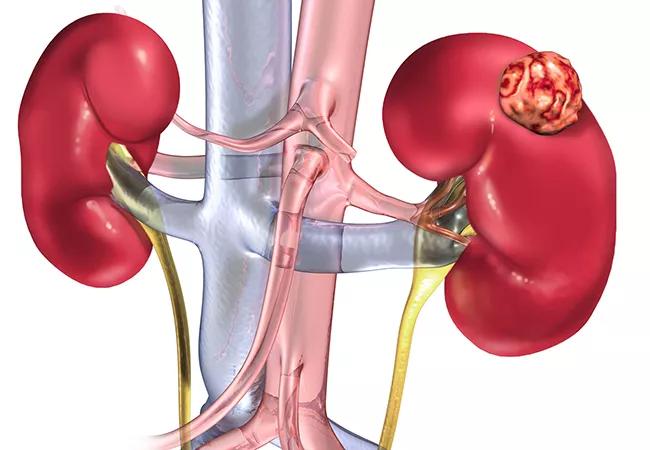
A new guideline from the American Urological Association provides clinicians with advice on best practices for managing patients with localized renal masses and cancers.The document is an update of two earlier guidelines, providing key evidence on evaluation and management of localized kidney cancer and surveillance after treatment, now merged into a single publication.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Developed under the leadership of experts from Cleveland Clinic and other leading kidney cancer centers, “Renal Mass and Localized Renal Cancer: Evaluation, Management, and Follow-up” takes a fresh look at such clinically important issues as:
“The new guidelines are based on a robust systematic review of the literature bringing all up to date as of late 2020,” says Steven C. Campbell, MD, PhD, chair of the AUA Renal Mass Guideline Panel and Vice Chairman of Urology at Cleveland Clinic. “This document provides clinicians with everything they need to know to take an evidence-based approach to evaluation and management of patients with localized kidney cancer and renal masses.”
To identify the literature to be reviewed, the panel used the same key questions and search criteria as for the Renal Mass and Localized Renal Cancer guidelines published in 2013 and 2017. The result was a “deep dive” into evidence in that area, spanning from January 1, 1997, through October 2020, and the capture of several additional studies.
In the process the panel merged the Renal Mass and Localized Renal Cancer guideline with a separate guideline on Follow-Up for Clinically Localized Renal Neoplasms.
Advertisement
Strength of evidence ratings—grades A for high, B for moderate, and C for low—were assigned to the body of evidence for a particular treatment when the panel found that sufficient evidence existed in the literature. In the absence of sufficient evidence, the guideline provides additional information, in the form of Clinical Principles and Expert Opinions.
The guideline includes 45 statements: 13 on initial evaluation and diagnosis, 19 on management, and 13 on follow-up after intervention. “None of the changes are earth-shattering, but they are all important and clinically relevant,” says Dr. Campbell. “In most cases, we fine-tuned the statements and provided more granular and clinically useful information.”
One example is the statement on radical nephrectomy (RN), which includes specific criteria for performing the procedure in patients with a solid or Bosniak 3/4 complex cystic renal mass whenever increased oncologic potential is suggested by tumor size, RMB (if obtained), and/or imaging features suggesting infiltrative or locally advanced features. In this setting RN is preferable if all of the following criteria are met: (1) the tumor is high complexity and partial nephrectomy would be challenging even in experienced hands; (2) the patient does not have preexisting CKD or proteinuria; and (3) the patient has a normal contralateral kidney and the new baseline estimated glomerular filtration rate (eGFR) will likely be >45 mL/min/1.73m2 even if RN is performed. The panel also notes that PN should be considered if all of these conditions are not met, unless there are overriding concerns about the safety or oncologic efficacy of PN.
Advertisement
“Which patients should get RN has been a very controversial issue and European and NCCN guidelines leave it up to the surgeon to decide just based on whether PN is thought to be feasible,” says Dr. Campbell. “The AUA guidelines are the only ones that provide granular and concrete information to help clinicians make solid decisions about this important issue.”
Among the other updates of particular note to clinicians are recommendations for active surveillance and expert advice on the role of contrast-enhanced MRI. “The 2017 guidelines indicated that contrast-enhanced MRI was inappropriate for patients with severe CKD and a GFR < 30mL/min/1.73m2,” says Dr. Campbell, “but with newer group II and III gadolinium-based contrast media, the risk is lower and it is safe, and the guidelines’ recommendations were changed to acknowledge this.”
What is most important for clinicians to know about the guidelines is that they are just that: guidelines. “At Cleveland Clinic, we do a pretty good job of following the main tenets, and we treat as many or more patients with kidney cancer than just about any other hospital in the world,” says Dr. Campbell. “But the reality is that it’s not 100% adherence. These are general recommendations that need to be interpreted within the context of the patient in front of you, with all the complexities that individual presents.”
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors