National expertise and coordinated patient care
A new Cleveland Clinic Children’s clinic is available for pediatric patients with congenital bone marrow failure syndromes (BMFS) or acquired bone marrow failure diseases such as aplastic anemia.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Patients with congenital bone marrow failure syndromes have mutations in critical genes that affect fundamental cellular pathways responsible for the production of blood cells, such as DNA repair, telomere maintenance or proteostasis.
These mutations — which result in conditions such as Shwachman-Diamond syndrome, severe congenital neutropenia (Kostmann syndrome), Fanconi anemia, dyskeratosis congenita and Diamond-Blackfan anemia — affect many parts of the body, including the pancreas and skeletal system. Patients also face the risk of developing leukemia or other cancers.
“These conditions are difficult to diagnose and difficult to manage and they often require multiple specialists,” says Seth Corey, MD, MPH, Pediatric Hematology Oncology and Blood and Marrow Transplantation, Cleveland Clinic. “The idea is to identify for each particular patient what his or her needs are and to provide one-stop shopping so the patient’s healthcare can be provided efficiently and accurately.”
Dr. Corey, who directs the clinic, came to Cleveland Clinic in 2018 from Virginia Commonwealth University and Children’s Hospital of Richmond. He says he was excited to join the staff and work with Jaroslaw Maciejewski, MD, PhD, Chair of Translational Hematology and Oncology Research. Dr. Maciejewski studies the development of BMFS and their molecular genetics.
“Through my collaboration with Dr. Maciejewski, Cleveland Clinic provides a unique center of expertise for congenital and acquired bone marrow failure syndromes in children and adults,” says Dr. Corey. “Our laboratories also collaborate to advance our understanding of these disorders with the goal of making healthier lives.”
Advertisement
The new monthly outpatient bone marrow failure clinic is located on the main campus and offers patients a range of specialists in BMFS — from genetic counselors and dentists to pulmonologists, oncologists, hematologists, cardiologists, plastic surgeons and others. The clinic offers patients a variety of treatments, including immunosuppresants, blood transfusions, hormones, growth factors and stem cell transplants.
The clinic also benefits from access to the latest clinical trials and the active research of physician scientists across Cleveland Clinic, including Drs. Corey and Maciejewski.
Dr. Corey’s lab is developing a zebrafish model to study Shwachman-Diamond syndrome (SDS), which affects about 1 in 70,000 live births. Using CRISPR/Cas9 editing, his lab has developed several strains of zebrafish that closely phenocopy human SDS. “The zebrafish copy all the features of SDS,” says Dr. Corey. “They’re small, neutropenic and have pancreatic and skeletal problems.”
He and his staff are now trying to determine which other genes cooperate with the SDS mutant gene to cause SDS patients to develop leukemia. The risk of developing leukemia and other cancers underscores the importance of a specialized clinic to patients with congenital BMFS. Using genomic sequencing and careful monitoring, Dr. Corey attempts to prevent cancer or detect it at an early stage in the clinic’s pediatric patients. He also hopes to better understand the mechanism that leads to cancer development.
His research investigates the mechanisms that underlie bone marrow failure such as the TP53 gene and its protein pathway. “TP53 plays a critical role in these disorders,” says Dr. Corey. “And the more we can characterize TP53 and its targets as culprits, the more we can understand what’s going on and how to ameliorate these conditions.”
Advertisement
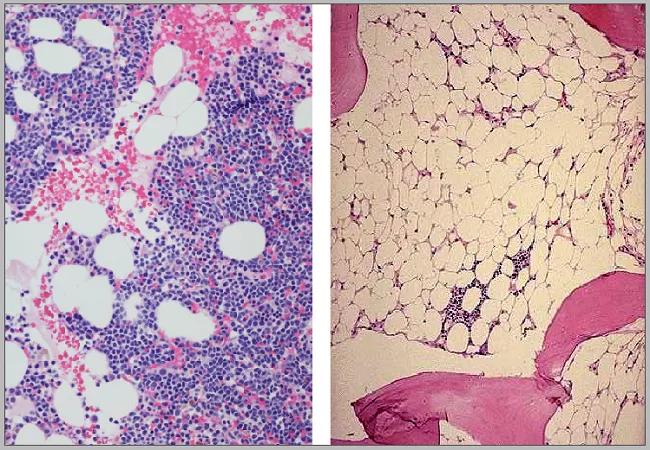
Feature image: Normal (left) and aplastic marrow.
Advertisement
Advertisement

Combining advanced imaging with targeted therapy in prostate cancer and neuroendocrine tumors

Early results show strong clinical benefit rates

The shifting role of cell therapy and steroids in the relapsed/refractory setting

Radiation therapy helped shrink hand nodules and improve functionality

Standard of care is linked to better outcomes, but disease recurrence and other risk factors often drive alternative approaches

Phase 1 study demonstrates immune response in three quarters of patients with triple-negative breast cancer

Multidisciplinary teams bring pathological and clinical expertise

Genetic variants exist irrespective of family history or other contributing factors