Cleveland Clinic’s Pituitary Tumor Center presents opportunity for research with large patient volume
A recent study has identified several factors that determine clinical outcomes in patients with acromegaly. The study looked at the clinical and hormonal profiles, co-morbidities, treatments, pathology and clinical outcomes of patients who were diagnosed with acromegaly at Cleveland Clinic over the past 15 years. The retrospective study was published in Clinical Diabetes and Endocrinology.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
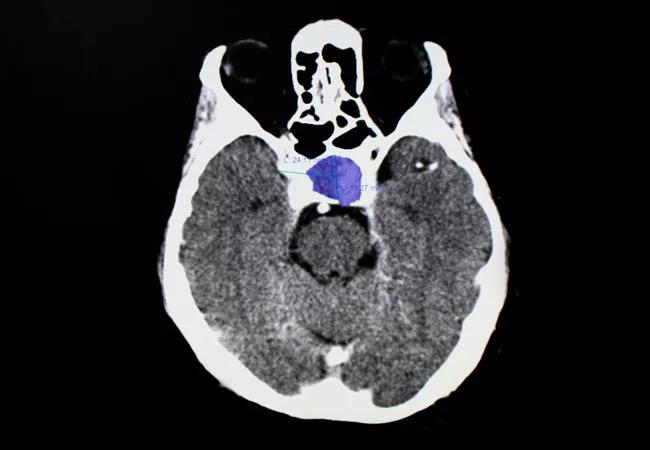
Although rare, acromegaly is characterized by excess growth hormone (GH) and insulin-like growth factor 1 (IGF-1) levels. The elevated IGF-1 levels cause somatic growth and metabolic effects, with increased morbidity and mortality, especially when the IGF-1 levels remain persistently high. Patients with suspected acromegaly are diagnosed with biochemical tests including random serum IGF-1 and GH level following a glucose load. A pituitary magnetic resonance imaging (MRI) is performed to assess for evidence of an adenoma, and surgical resection is the standard of care.
“I felt that because Cleveland Clinic is a large pituitary tumor center of excellence, we had a unique opportunity to report some very large numbers of patients and outcomes,” says Divya Yogi-Morren, MD, Medical Director of the Pituitary Tumor Center in Cleveland Clinic’s Endocrinology and Metabolism Institute and lead author on the study. “Even though it is typically a rare disease, we see a lot of it because of our high clinical volume. In fact, we have the patient volume to support two dedicated pituitary surgeons.”
The study was a 15-year retrospective chart review that looked at patients from 2003 to 2018. It included a total of 136 patients (62 men and 74 women) who were diagnosed at a mean age of 48.1 ± 13.8 years. “We looked at several factors including their clinical history, their hormone levels, what treatment they received and what their surgical pathology was after they had surgery done. Then, we followed them to see how they did and what their clinical outcomes were,” says Dr. Yogi-Morren.
Advertisement
A large majority of patients (89.6%) reported musculoskeletal complaints, compressive symptoms were reported by 65.6% of patients and 45.2% of patients reported hypogonadism. The most common comorbidities presented by patients were hypertension (56.7%), obstructive sleep apnea (47.5%) and diabetes mellitus (44.4%). The median IGF-1 level at diagnosis was 769.0 ng/mL with median baseline GH level of 8.2 ng/mL (0.17 to 808.12 ng/mL), and median nadir 2-h post-OGTT GH level of 4.4 ng/mL (0.2 to 330.0 ng/mL).
Most patients were discovered to have a macroadenoma (82.2%), with median tumor dimensions of 16.0 (antero-posterior) × 16.0 (transverse) × 14.0 (craniocaudal) mm. Complete visible tumor resection during initial surgery was achieved in 87 patients (64.0%). Complete response to surgery alone was found in 61 patients (70.0%) and 31 out of the 65 patients (47.7%) who received additional post-surgical medications and/or radiation therapy achieved complete response. Ninety-two patients achieved eventual complete response by documented normalization of IGF-1 levels. However, the researchers found that a higher IGF-1 level at diagnosis (P = 0.024) and cavernous sinus invasion (P = 0.028) were predictors for a failure to respond to surgery.
“The majority of these were macroadenomas—they were very large tumors,” explains Dr. Yogi-Morren. “It is also interesting that they were plurihormonal, meaning that they were not just producing growth hormone as expected in acromegaly, but they were also producing some other type of pituitary hormone. Most of them were treated effectively with surgery alone or surgery with some kind of adjuvant medical therapy or radiation.” Dr. Yogi-Morren also notes that patients who had sparsely granulated tumors did not respond as well to either surgery or to treatment.
Advertisement
Dr. Yogi-Morren has identified a few areas where future research should focus. “One of the most interesting findings coming out of this study is that it seemed that patients who had sparsely granulated tumors are the ones who did not respond as well to either surgery or to treatment,” she says. “That is an area we will be looking at in our future studies. It seems like that is one factor that determines why certain types of tumors do not respond as well to surgery and/or medication and radiation.”
Advertisement
Advertisement

Pheochromocytoma case underscores the value in considering atypical presentations

Advocacy group underscores need for multidisciplinary expertise

A reconcilable divorce

A review of the latest evidence about purported side effects

High-volume surgery center can make a difference

Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D

Patients spent less time in the hospital and no tumors were missed

A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications