Findings add more to the discussion about how to classify and treat obesity

Obesity is a public-health threat that affects close to half of the United States population. While lifestyle interventions, such as reducing caloric intake and increasing physical activity, make up the primary prevention and treatment methods, they have limitations to their effectiveness. To improve success rates, anti-obesity medications (AOMs) can be used in tandem with lifestyle interventions. The large majority of AOMs work modifying the appetite set-point in the brain helping patients to feel less hungry. However, even though there is extensive data on the effectiveness of AOMs, data regarding their use in workplace wellness plans are lacking, and coverage of AOMs by US private employers is very limited.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
A recent study appearing in JAMA Network Open examined the effectiveness of combining AOMs with a comprehensive, interdisciplinary employer-based weight management program (WMP) against the effectiveness of the WMP alone in terms of weight loss, treatment adherence. It found that clinically meaningful superior mean weight loss was achieved when access to AOMs was provided in the real-world setting of an employer-based WMP, compared to the WMP alone.
In the study, 200 randomized subjects were predominately (88.5%) female, had a mean (SD) age of 50.0 (10.29) years and baseline weight of 105.0 (19.01) kg. For the primary “intention-to-treat” cohort, estimated mean (SE) weight loss was -7.7% with WMP plus AOM. The cohort of subjects who did not receive AOMs saw a weight loss of -4.2%. The estimated percentage of subjects achieving ≥5% weight loss was 62.5% for WMP plus AOM versus 44.8% for WMP only. There were no meaningful differences in patient-reported work productivity or limitation measures were observed.
“More long-term research is needed in real-world, employer-based settings to evaluate the costs and benefits of anti-obesity medications and their use in conjunction with workplace wellness plans,” says Bruce Rogen, MD, MPH, a staff physician in Cleveland Clinic’ Internal Medicine and Geriatrics Department and one of the study’s authors.
“This manuscript shows that in the real-world, we are able to help our patients lose a very significant amount of weight,” says Bartolome Burguera, MD, PhD, the Chairman of Cleveland Clinic’s Endocrinology & Metabolism Institute and senior author of the study. “We know that losing more than 5% of original body weight already has a significant impact on improving quality of life, improving blood pressure, blood glucose and individual’s sense of well-being. In this paper, we were very close to getting 10% weight loss, which is superb.”
Advertisement
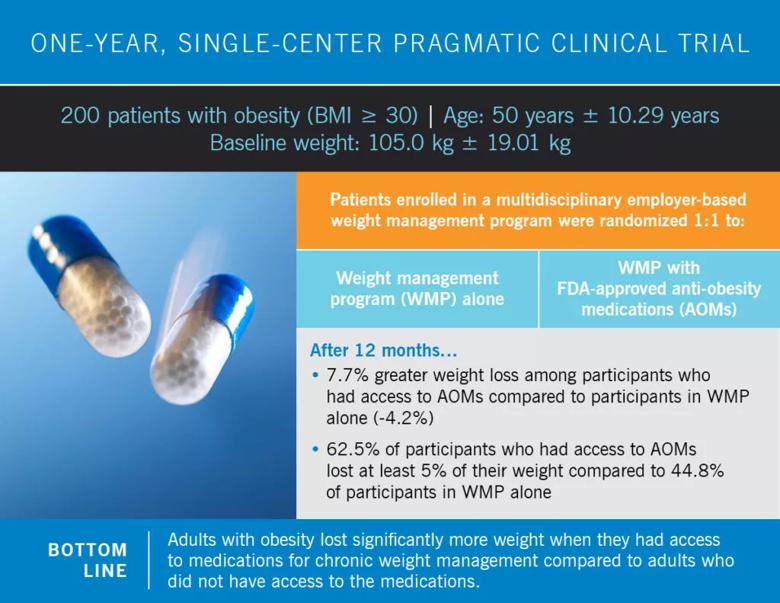
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/5b0b0e74-445b-448a-8ecb-258bae8cbfbd/21-EMI-2161008-CQD-Anti-obesity-medication-VA-1024x791_jpg)
Dr. Burguera says one of the main reasons for conducting the study was because of the need to shift the philosophy towards obesity. He argues that many people still feel obesity is a self-inflicted disease, and the solution is just to eat less and exercise more.
“Physicians, in general, don’t want to treat obesity,” says Dr. Burguera. “There is still a common bias against obesity that it’s a self-inflicted. We need to change that mentality. Health systems are not prepared to deal with obesity. At Cleveland Clinic, we have more than 9,000 patients coming to Cleveland Clinic every day with a BMI over 35. They come for many reasons, including heart disease, hip issues or depression, which are directly correlated to their obesity. We are working hard with strong support from our leadership, to make sure the primary problem here—obesity—is being diagnosed and treated.”
In order to overcome this disconnect, Cleveland Clinic treats obesity through an interdisciplinary team integrated by obesity specialists, dieticians, exercise physiologists, psychologist and bariatric surgeons. Physicians within each of Cleveland Clinic’s institutes are consulted to address the specific obesity comorbidities and work together to improve obesity care.
Dr. Burguera believes that AOMs can be an effective tool for helping patients lose weight. However, one of the primary factors affecting its accessibility is cost — AOMs are generally not covered by insurance. Dr. Burguera sees this as a symptom of treating obesity as a condition rather than a disease. “In general, employers feel that they cannot add medication that costs $100 or $150,” he says. “But considering that almost 50% of the population has obesity, they’re already paying for the consequences of obesity. They’re paying for the blood pressure medication, the diabetes medications, the antidepressants, the osteoarthritis medications and all of the other complications. It’s time to start considering obesity as a chronic disease. Increasing physical activity and reducing issues related to stress and sleep are beneficial, but in many circumstances, it is also important to reducing appetite with AOMs to help patients feel less hungry, have more control over their hunger and make better choices.
Advertisement
Advertisement

Advocacy group underscores need for multidisciplinary expertise

A reconcilable divorce

A review of the latest evidence about purported side effects

High-volume surgery center can make a difference

Advancements in equipment and technology drive the use of HCL therapy for pregnant women with T1D

Patients spent less time in the hospital and no tumors were missed

A new study shows that an AI-enabled bundled system of sensors and coaching reduced A1C with fewer medications

Association revises criteria for the diagnosis and resolution of severe conditions