New procedure eliminates volvulus risk
A novel surgical procedure based upon new insights into the embryologic defects of gut malrotation has proven to be safe and effective, according to a recent Cleveland Clinic study published in Annals of Surgery.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
“Our aim with this study, the largest of its kind worldwide, was threefold,” says Kareem Abu-Elmagd, MD, PhD, Director of Cleveland Clinic’s Center for Gut Rehabilitation and Transplantation and lead author of the study. “First, we defined the clinicopathologic spectrum of such a life-long disorder among all ages. Second, we addressed the incidence of midgut loss and the associated risk factors with special reference to the efficacy of gut transplantation particularly in infants and children. Last but foremost, we introduced the new gut malrotation correction (GMC) surgery as an effective and safe procedure in both children and adults.”
The clinical significance of inborn midgut anomalies was established in the 1920s, followed by the introduction of Ladd’s procedure in the 1930s. The lifesaving procedure untwists volvulus and releases Ladd’s bands to treat duodenal obstruction with widening of the mesentery to reduce risk of recurrent volvulus. Despite a few modifications over the last century, development of volvulus continued to threaten the life of some of these patients regardless of age, with worsening digestive symptoms among the adult population.
“Pediatric and adult gastroenterologists should be aware of the new insights into the pathophysiology and clinical presentation of gut malrotation,” says Dr. Abu-Elmagd. “The congenital disorder is not just a simple morphologic anomaly but it is associated with a defective mesenteric and neuroenteric embryonic development.”
In addition to the risk of volvulus, the new, comprehensive study confirms the clinicopathologic heterogeneity of the syndrome with subtle and often overlooked symptoms in a considerable number of patients. The newly defined gut malrotation syndrome (GMS) was diagnosed in nearly half of the study patients with disabling digestive symptoms.
Advertisement
“The outlook for gut malrotation patients who develop catastrophic midgut loss has improved significantly with the introduction of gut transplantation (GT) and autologous gut reconstruction (AGR),” notes Dr. Abu-Elmagd. “This study with a 30 year follow-up is a testimony of the therapeutic efficacy of these integrative surgeries in both children and adults with the best outcome among infants. Accordingly, rather than recommending comfort care for newborn and infants with midgut loss, neonatologists and pediatricians should share these encouraging results with the parents as an important part of the decision-making process.”
Dr. Abu-Elmagd adds, “With our three decades of experience in the establishment of the field of gut rehabilitation and transplantation, the concept of the new gut malrotation correction (GMC) surgery has evolved; we believe this procedure will be practice changing and begin a new paradigm in the standard of care.”
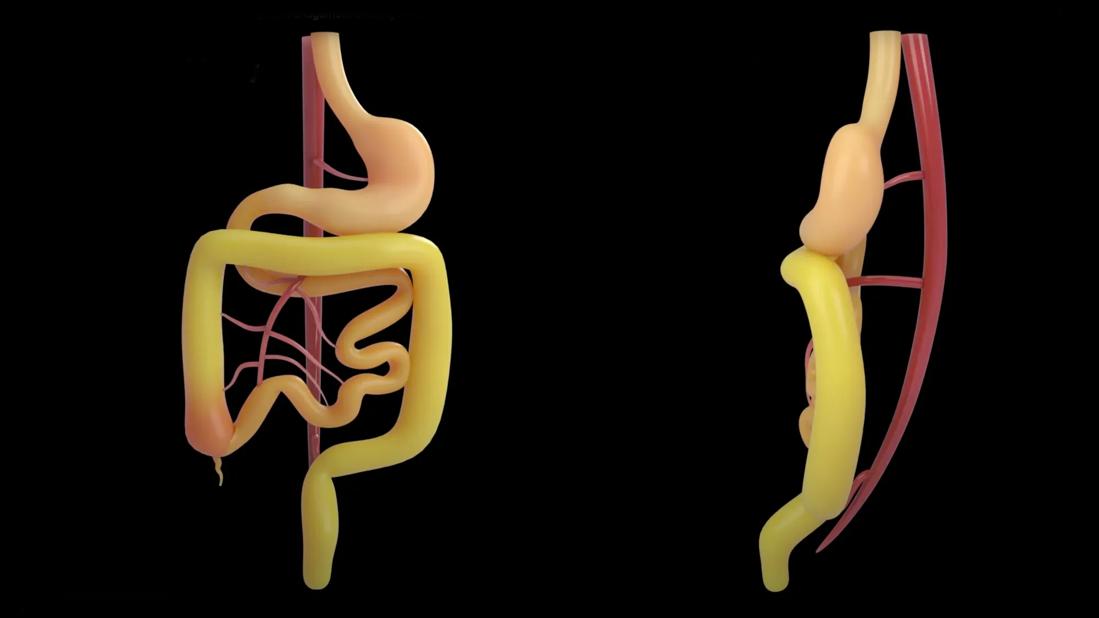
GMC involves completing the embryonic, 270-degrees-counterclockwise rotation and establishing all mesenteric attachments. The procedure aims to alleviate the disabling gastrointestinal symptoms and prevent volvulus. “Pediatric and adult digestive surgeons should know that the operation is simple, safe and easy to perform in both children and adults,” Dr. Abu-Elmagd confirms.
“Our aim with this study, the largest of its kind worldwide, was threefold,” says Kareem Abu-Elmagd, MD, PhD, Director of Cleveland Clinic’s Center for Gut Rehabilitation and Transplantation and lead author of the study. “First, we defined the clinicopathologic spectrum of such a life-long disorder among all ages. Second, we addressed the incidence of midgut loss and the associated risk factors with special reference to the efficacy of gut transplantation particularly in infants and children. Last but foremost, we introduced the new gut malrotation correction (GMC) surgery as an effective and safe procedure in both children and adults.”
Advertisement
The clinical significance of inborn midgut anomalies was established in the 1920s, followed by the introduction of Ladd’s procedure in the 1930s. The lifesaving procedure untwists volvulus and releases Ladd’s bands to treat duodenal obstruction with widening of the mesentery to reduce risk of recurrent volvulus. Despite a few modifications over the last century, development of volvulus continued to threaten the life of some of these patients regardless of age, with worsening digestive symptoms among the adult population.
“Pediatric and adult gastroenterologists should be aware of the new insights into the pathophysiology and clinical presentation of gut malrotation,” says Dr. Abu-Elmagd. “The congenital disorder is not just a simple morphologic anomaly but it is associated with a defective mesenteric and neuroenteric embryonic development.”
In addition to the risk of volvulus, the new, comprehensive study confirms the clinicopathologic heterogeneity of the syndrome with subtle and often overlooked symptoms in a considerable number of patients. The newly defined gut malrotation syndrome (GMS) was diagnosed in nearly half of the study patients with disabling digestive symptoms.
“The outlook for gut malrotation patients who develop catastrophic midgut loss has improved significantly with the introduction of gut transplantation (GT) and autologous gut reconstruction (AGR),” notes Dr. Abu-Elmagd. “This study with a 30 year follow-up is a testimony of the therapeutic efficacy of these integrative surgeries in both children and adults with the best outcome among infants. Accordingly, rather than recommending comfort care for newborn and infants with midgut loss, neonatologists and pediatricians should share these encouraging results with the parents as an important part of the decision-making process.”
Advertisement
Dr. Abu-Elmagd adds, “With our three decades of experience in the establishment of the field of gut rehabilitation and transplantation, the concept of the new gut malrotation correction (GMC) surgery has evolved; we believe this procedure will be practice changing and begin a new paradigm in the standard of care.”
GMC involves completing the embryonic, 270-degrees-counterclockwise rotation and establishing all mesenteric attachments. The procedure aims to alleviate the disabling gastrointestinal symptoms and prevent volvulus. “Pediatric and adult digestive surgeons should know that the operation is simple, safe and easy to perform in both children and adults,” Dr. Abu-Elmagd confirms.
Video content: This video is available to watch online.
View video online (https://www.youtube.com/embed/07_xTYr5IOM?feature=oembed)
Gut Malrotation Surgery
The study includes a total of 500 patients with gut malrotation. Fifty-five percent of patients were children at the time of diagnosis. In patients with midgut loss (41%), GT was done in 85%, and 7% had AGR. The new procedure was performed in 80 patients with intact gut and disabling symptoms.
“With the longest follow-up ever reported in the literature, we were able to identify the cumulative risk and predictors of midgut loss such as volvulus, prematurity, gastroschisis and intestinal atresia,” says Dr. Abu-Elmagd. “We also tracked the outcomes in patients who received GT and AGR. One of the crucial points of the study was defining malrotation as a disorder that presents across the lifespan that should be successfully treated.”
Eighty patients underwent GMC surgery including children. There was no single example of technical complications with uneventful postoperative recovery. As expected, the long-term survival of the patients who underwent GMC exceeded those who lost their midgut and underwent AGR and/or GT. All GMC patients are currently alive with no recurrent or de novo volvulus. Within up to 10 years, all patients continued to experience significant improvement in the self-reported outcomes gastrointestinal symptom scales with better quality of life.
Advertisement
“With these encouraging outcomes, we believe that GMC should be offered to all patients with gut malrotation,” says Dr. Abu-Elmagd. “Our next goal is to see the establishment of a CPT code and training for both pediatric and adult digestive surgeons as part of a surgical curriculum."
In 2023, Dr. Abu-Elmagd and Salvadore Navarette, MD began taking a laparoscopic approach with the procedure. Noting that the procedure is almost identical to the surgical approach, there are several benefits to both the surgeon and the patient by doing this laparoscopically. Since the laparoscopic approach is less invasive, it means fewer risks and an easier recovery for the patient. It also takes less time to perform the procedure this way. Drs. Abu-Elmagd and Navarette note that while they have had success with the laparoscopic approach, they continue to perfect it and optimize patient selection.
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years