Research highlights promising outcomes for treating recurrent and metastatic cases
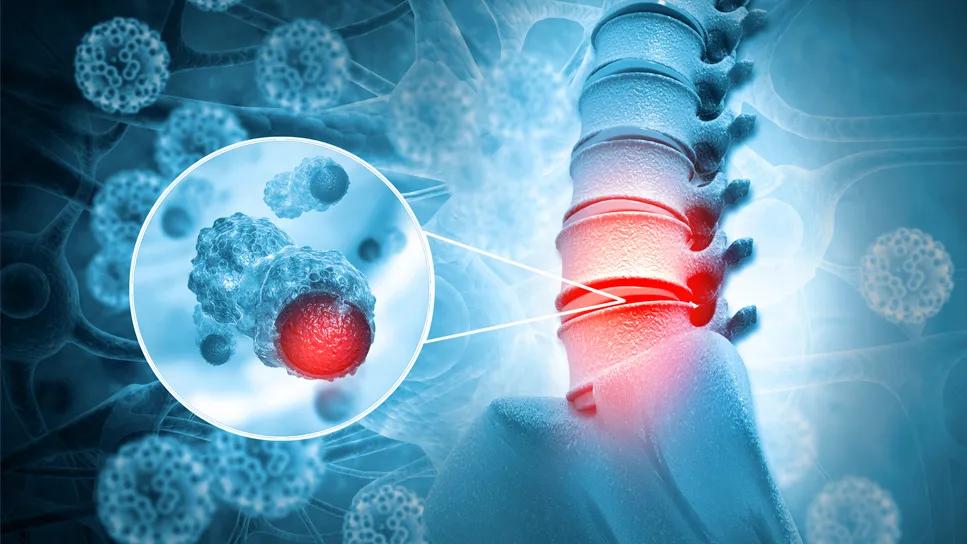
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3b30c93f-6d5a-48e5-9d98-dc8f8525059c/sbrt-for-metastatic-osteosarcoma-1335843615)
Spine cancer
New analysis showed that stereotactic body radiation therapy (SBRT) is both a safe and effective treatment for recurrent and metastatic osteosarcoma, with a one-year cumulative local failure (LF) rate of 13.6%.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Data from this study, presented during the 2024 American Society of Radiation Oncology (ASTRO) Annual Meeting, also suggests that SBRT targeting spinal lesions was associated with the highest risk of local recurrence, underscoring the need to modify treatment strategies for tumors near critical structures.
Treatment of osteosarcoma, a rare, radioresistant malignancy, can prove challenging, particularly in achieving locoregional control. Stereotactic body radiation therapy has emerged as a potential option, offering high-dose precision radiation to target recurrent or metastatic tumors. However, radiation is typically not considered a standard treatment for osteosarcoma.
Despite its growing use, especially in sarcoma cases, there remains limited data on its impact, particularly in pediatric patients, according to study author Jenna Kocsis, MD, a resident physician in the Department of Radiation Oncology at Cleveland Clinic. Dr. Kocsis initiated the current study, alongside her mentor Dr. Erin Murphy and colleagues, to address this knowledge gap.
The Cleveland Clinic-led research team reviewed practice patterns, outcomes, toxicity and patterns of failure when treating osteosarcoma patients with stereotactic body radiation therapy.
Dr. Kocsis and colleagues reviewed an IRB-approved registry of patients who underwent SBRT for recurrent or metastatic sarcoma between 2015 and 2023. Patients were evaluated for local control (LC), overall survival (OS) and toxicity.
Local failure rates were determined using cumulative incidence analysis, while overall survival (OS) rates were estimated using actuarial analysis. Competing risk regression was employed to identify factors linked to LF. Dosimetric evaluation was used to assess local failure patterns.
Advertisement
In-field failures (IFF) were classified when 80% or more of the recurrent tumor volume was within the 95% prescription isodose line (IDL), marginal failures (MF) when 20%-80% of the volume was within the IDL, and out-of-field failures (OOF) when less than 20% of the recurrent tumor volume was within the IDL.
The registry review identified 27 eligible patients with a total of 71 lesions treated and a median age of 18.1 years. Of those, six patients were alive at the time of analysis. The median follow-up time was 5.9 months.
Of the 71 lesions treated, 47 (66.2%) were osseous, 12 (16.9%) were parenchymal and 12 (16.9%) involved soft tissue. Among the 47 osseous lesions, 24 (51.1%) were located in the spine, while 23 (48.9%) were in an extremity or pelvis. Of the 24 spinal lesions, 10 (41.7%) had epidural involvement.
The median radiation dose was 40 Gy in five fractions, with the most common fractionation schedules being 40 Gy in five fractions (45.1%) and 21 Gy in three fractions (12.7%). Concurrent therapies, such as chemotherapy, targeted agents or radionucleotides, were administered in 53 cases (74.6%), with 32 lesions (60.4%) receiving concurrent chemotherapy.
A total of 11 local failures (15.5%) were observed, and data showed that the six- and 12-month cumulative incidence of LF was 10.3% and 13.6%, respectively. Of the local failures, there were four IFF, three MF and four OOF. Additionally, there were seven spine local failures, and five (71.4%) of them failed with epidural disease. Overall survival rates were 87.5% at six months and 64.1% at one year.
Advertisement
Acute toxicity was low, with only four cases of grade 2 side effects, such as esophagitis, pneumonitis and increased pain. No patients experienced grade 3 or higher acute toxicity, and only one patient had a significant late complication, requiring sacroplasty nine months after SBRT.
This research demonstrates that SBRT is both safe and effective for recurrent and metastatic osteosarcoma. While local failures were observed, they were evenly distributed across different failure types (IFF, MF, OOF). The analysis suggests that spine lesions, especially those near critical structures like the epidural space, have a higher risk of recurrence.
These findings highlight the need for strategy adjustments when treating tumors in sensitive anatomical areas. SBRT offers a promising treatment option for osteosarcoma, though further research is needed to optimize its application.
“Our study sheds light on another potential treatment approach for this patient population,” notes Dr. Kocsis. “Children with recurrent or metastatic disease don’t always want to undergo surgery, which can be quite disruptive and have a significant impact on their daily life and cause delays in their systemic therapy. If radiation can offer comparable outcomes and provide better quality of life, it could be an effective—and less invasive—option for our patients.
“And that is our goal, to determine the role of radiation in the treatment paradigm of recurrent and metastatic osteosarcoma,” she concludes. “That is not to say that there still isn’t a need for surgical intervention. Surgery is a great option and remains the gold standard. It is more about making sure that patients and their families and physicians can make an informed decision on what’s best for the individual patients. Sometimes it's surgery, but sometimes it can be radiation as well.”
Advertisement
Hear our recent podcast about treating recurrent osteosarcoma with SBRT.
Advertisement
Advertisement
Study also finds that 26% of children with cancer have mutations in DNA repair genes
Biologic approaches, growing implants and more
Case study of radial-to-axillary nerve transfer for tumor-related deltoid nerve injury
An update on the technology from the busiest Gamma Knife center in the Americas
Tapping into motivational interviewing to guide behavioral change
Complex disease requires a comprehensive approach
Rare genetic disorder prevents bone mineralization
Radiation oncology department finds weekly plan of care meetings have multiple benefits