Study points to proper surveillance and additional research

When it comes to colorectal cancer, there’s good news and there’s bad news. The good news is that the incidence of colorectal cancer in adults age 50 and older in the U.S. is decreasing. The bad news is that the incidence and mortality rates for colon cancer in young adults under age 50 are increasing. In 2030, JAMA Surgery projects that the incidence rates for colon and rectal cancers will increase by 90 percent and 124 percent, respectively, for patients between 20 and 34 years of age.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
In addition to understanding why colorectal cancer rates are increasing in young adults, physicians want to know how to manage these patients once polyps have been detected and removed. Their goal is to decrease the risk of cancer and utilize resources appropriately. However, there are no published guidelines for colorectal cancer screening or alterations in surveillance colonoscopy for young adults who have had polyps.
To help improve patient care, Cleveland Clinic recently published one of the largest case-control studies to assess the polyp characteristics and follow-up findings in patients under age 40 and compare them to the findings in adults over age 50. Under the leadership of Carol Burke, MD, Vice Chair of Cleveland Clinic’s Department of Gastroenterology and Hepatology, the study revealed that 38 percent of young adults who had polyps found on colonoscopy had high-risk polyps. Results of the study also suggest that the polyp findings on follow-up colonoscopy in young people can be predicted by baseline polyp features.
While the cause of early-onset colorectal cancer is unknown, many factors are conjectured to contribute to this epidemic, including the following:
“These risk factors do not completely explain the trends seen in young-onset colorectal cancer incidence, especially since the risk factors are also present in older individuals,” notes Dr. Burke. “Certainly, the use of colorectal cancer screening in adults over age 50 and the removal of their polyps before they become cancerous contributes to the noted decrease in the colon cancer-related incidence and mortality rates,” she explains. “In addition, some medications frequently taken by older individuals (e.g., statins, aspirin and anti-inflammatories) may also reduce risk.”
Advertisement
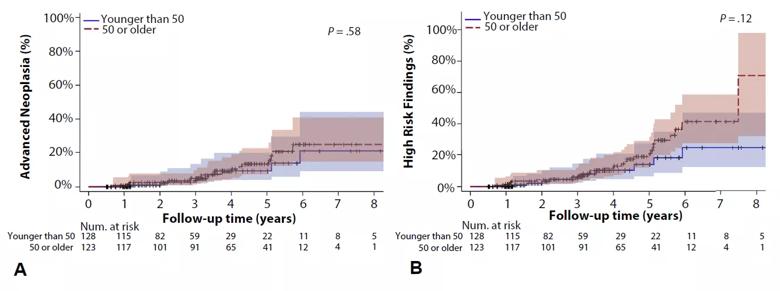
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/71063778-03f7-494b-9213-f832c7956f88/Figure1_Time_toOccurrence_A_metachronous-advanced-neoplasia_B_High-riskPolypFeaturesByAge_png)
Figure. Time to occurrence of (A) metachronous advanced neoplasia and (B) high-risk polyp features by age cohort (Source: Gastrointestinal Endoscopy/Cleveland Clinic).
Dr. Burke’s team studied a group of 128 patients with polyps who were less than 40 years old and who had a follow-up colonoscopy. The study revealed that 38 percent of young adults had high-risk polyps, including 35 percent with advanced adenomas (> 9 mm or with any villous features or high-grade dysplasia).
When compared to a cohort of patients over 50, the proportion of patients with high-risk polyps was similar to the risk seen in the older cohort of mainly average-risk individuals. The team was surprised at the high prevalence of advanced neoplasia and high-risk polyp characteristics that were found in young adults. “If these findings are corroborated in larger studies, they may help explain the growing epidemic of young-onset colorectal cancer and alter the age at which we begin colorectal screening,” says Dr. Burke.
While screening guidelines may change in the future, the study provides some evidence to suggest that postpolypectomy surveillance guidelines may be the same for both younger and older adults. “When stratifying risk based upon baseline polyp characteristics, in our small study, young adults with high-risk features were no more likely than older adults to have an advanced polyp detected during a follow-up colonoscopy,” explains Dr. Burke. “Thus, we recommend following the same surveillance guidelines that are derived from studies involving older adults.” These guidelines include a five- to 10-year interval for patients with low-risk polyp features (1–2 small tubular adenomas) and a three-year interval for those with high-risk features (advanced pathology; large or > 2 adenomas).
Advertisement
Regardless of age, physicians should be diligent about recommending a diagnostic colon evaluation when unexplained colorectal symptoms are involved. “While abdominal discomfort and changes in bowel habits are quite common, iron deficiency anemia or rectal bleeding may indicate large polyps or colorectal cancer,” notes Dr. Burke. “Doctors should never dismiss rectal bleeding as hemorrhoids just because the patient is young.” Young patients should be proactive in pursuing an assessment of their symptoms.
Larger studies are needed to develop screening guidelines for young adults and further characterize polyp behavior. “Considering our limited healthcare resources, it’s important to identify the most accurate, cost-effective colorectal cancer screening strategy for young adults,” explains Dr. Burke. In addition, researchers will need to investigate the microbiome of young adults with polyps to see if there is any connection between the polyps and viruses in the intestinal tract.
A colorectal cancer screening program for young adults could involve testing that’s simpler than a colonoscopy. “In our study, 68 percent of adenomas in young patients were in the distal colon versus 49 percent in adults age 50 or older. Screening with a flexible sigmoidoscopy and a fecal immunochemical test may be a strategy for colorectal cancer screening in young individuals,” explains Dr. Burke. “I believe that most young patients would prefer a five- to 10-minute sigmoidoscopy over a colonoscopy — since it doesn’t require bowel prep or sedation.”
Advertisement
Advertisement

Benefits of neoadjuvant immunotherapy reflect emerging standard of care

Multidisciplinary framework ensures safe weight loss, prevents sarcopenia and enhances adherence

Study reveals key differences between antibiotics, but treatment decisions should still consider patient factors

Key points highlight the critical role of surveillance, as well as opportunities for further advancement in genetic counseling

Potentially cost-effective addition to standard GERD management in post-transplant patients

Findings could help clinicians make more informed decisions about medication recommendations

Insights from Dr. de Buck on his background, colorectal surgery and the future of IBD care

Retrospective analysis looks at data from more than 5000 patients across 40 years