Taking virtual reality-integrated technology from silver screen to clinical laboratory
In 2008, the National Academy of Engineering identified 14 Grand Challenges for Engineering that, if addressed, could be game changers in health and quality of life. One of those challenges was the integration of virtual reality (VR) into medicine — a pursuit in which progress has been incremental at best. A major barrier has been the locomotion problem: individuals using traditional VR often report nausea due to a disconnect between visual and somatosensory information.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Recently scientists at Cleveland Clinic have developed a solution to the locomotion problem and have created a truly immersive VR experience. They are initiating research to use their platform to understand and better treat freezing of gait in patients with Parkinson’s disease (PD). Future research plans include use of the platform for early identification of PD and other neurodegenerative disorders in older adults.
The Infinadeck®, an omnidirectional treadmill (Infinadeck Corp., Rocklin, California), is an important component of the solution. Similar to treadmills in the home or fitness centers, it has a linear motion component. However, it also has a rotary motion aspect that moves in conjunction with the surface of the treadmill. This multipurpose treadmill was featured in the 2018 Steven Spielberg sci-fi movie Ready Player One.
“You can think of it as a treadmill on a thousand treadmills,” says Jay Alberts, PhD, staff in Cleveland Clinic’s Center for Neurological Restoration and Department of Biomedical Engineering, whose lab recently developed the new VR platform.
When paired with the algorithms of the treadmill’s computerized control system, the multiple belts are designed to keep the treadmill user in the center of the treadmill platform by constantly adjusting linear and rotary contributions. “It’s an elegant system that allows real walking while the patient moves through a virtual environment,” notes Dr. Alberts.
By producing constant linear and rotary adjustments as a result of user position, the platform overcomes the locomotion problem that often causes nausea. “A traditional VR environment may simulate movement in a way that involves changes in visual information — for example, that you’re going up or down on a roller coaster — without your somatosensory and vestibular systems having the same experience,” Dr. Alberts explains. “So there is a mismatch in sensory information in the brain that tends to trigger nausea in many people. The design of the omnidirectional treadmill allows a subject with a VR headset to experience the same somatosensory information and sensations that that they experience during real-world walking, which allows them to physically explore the virtual world they are in without experiencing nausea or similar discomfort.”
Advertisement
Eliminating nausea and immersing the patient in the virtual environment opens up countless clinical and healthcare research possibilities. Once a solution for the locomotion problem was imminent, Dr. Alberts and his team started building virtual environments that replicated conditions and situations that individuals with PD often reported were difficult.
The first virtual environment they developed was the Cleveland Clinic Virtual Grocery Store Task, in which a subject wearing a VR headset walks on the treadmill to navigate through a virtual grocery store. Importantly, subjects are able to walk down aisles as they would in a real store, doing everything from straight-line walking to making turns to turning directions as they reach for items on their shopping list (see video and figure below).
Video content: This video is available to watch online.
View video online (https://cdnapisec.kaltura.com/p/2207941/sp/220794100/playManifest/entryId/1_ie8zstwj/flavorId/1_5f3sgelj/format/url/protocol/https/a.mp4)
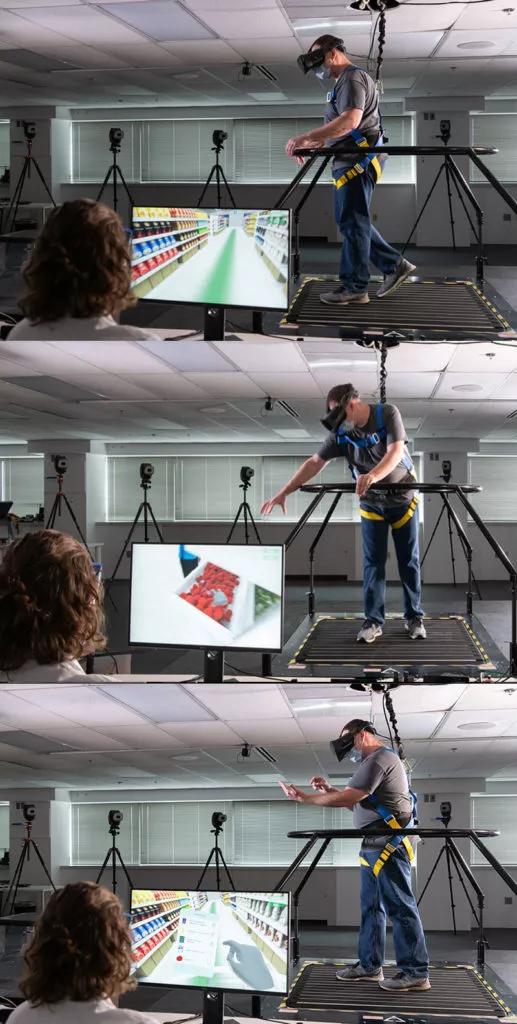
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/0353c84c-32e0-4f8d-96c9-48c96d2794d2/21-NEU-2225280-CQD-Inset-038-091-031-800x1583-1-517x1024_jpg)
Figure. A volunteer uses the VR platform to walk through a virtual grocery store, navigating aisles, reaching for items and checking off selections on a virtual mobile phone.
This is the first healthcare-related VR application that truly immerses patients in an environment that often results in freezing of gait or falls. Freezing is a debilitating symptom of PD that is difficult to treat, in part because it rarely is elicited during typical clinical visits. “It is difficult to treat a symptom that you cannot see,” notes Dr. Alberts.
Cleveland Clinic’s efforts with this new technology are the first of their type that Dr. Alberts is aware of in healthcare research and clinical practice. He says the efforts have three broad clinical goals.
Advertisement
Identifying and monitoring neurodegenerative disease. One is to use the VR platform to evaluate instrumental activities of daily living (iADLs) in older individuals at risk for conditions such as PD and Alzheimer’s disease (AD). iADLs are activities that enable an individual to live independently. In addition to requiring motor skills, they involve more significant cognitive skills than ADLs. Examples include cooking, house cleaning, taking medications, shopping, tending to personal finances and overseeing one’s own transportation outside the home.
“Good data show that a decline in iADLs may be a prodromal marker for PD and AD,” says Dr. Alberts. “If we could integrate virtual environment tasks using the omnidirectional treadmill into a clinical setting, we could likely identify these diseases before clinical onset of symptoms and be able to intervene earlier. The virtual tasks using the treadmill allow for assessment of iADLs in less time and using less space compared with assessment of an individual by an occupational therapist using some sort of mock grocery store or similar environment. The treadmill also enables subjective quantitative assessment of iADL function.” Brief iADL assessment using the technology could ultimately become part of geriatric patients’ annual examination, he notes.
Evaluating gait freezing to fine-tune PD therapy. A second and more near-term goal is to use the omnidirectional treadmill to evaluate freezing of gait in patients with PD with the aim of refining their deep brain stimulation (DBS) programming and/or PD medication regimens.
Advertisement
“People with PD tend to freeze and fall when they are doing a challenging task that involves dual motor and cognitive components,” explains Dr. Alberts. In a soon-to-launch trial involving 15 patients with PD, he and Kenneth Baker, PhD, of Cleveland Clinic’s Center for Neurological Restoration are going to do neurophysiologic monitoring of the subthalamic nucleus while patients complete the grocery store task and a home environment task on the treadmill. Their aim is to identify the neural signature of freezing-of-gait episodes in these patients. “We expect to then be able to use DBS electrodes to target and change a patient’s neural activity and better treat freezing of gait and other forms of postural dysfunction,” he says. The work just received a three-year, $2 million grant from the Michael J. Fox Foundation for Parkinson’s Research.
Safely enhancing rehabilitation therapy. A third initial goal is to use the technology to safely step up rehabilitation therapy for patients with various conditions, from PD to stroke to recovery from orthopaedic surgery. “VR environments for harnessed patients on an omnidirectional treadmill allow you to safely tax and test patients’ gait and postural stability in ways not otherwise possible,” Dr. Alberts says. The subjective nature of quantification by the treadmill system also offers distinctive value for monitoring a patient’s rehab progress.
Dr. Alberts says new virtual environments for the treadmill system will introduce simulations of stressful situations likely to trigger freezing of gait or similar episodes, such as the need to walk through a rapidly closing sliding glass door.
Advertisement
He adds that while individuals with PD, AD and stroke are obvious initial patient populations that stand to benefit from this technology, additional applications are certain. “Some of the same types of factors that trigger freezing of gait and falls in PD may trigger seizures in people with epilepsy,” he notes, “so we are working with our epilepsy colleagues to determine potential standard approaches or VR protocols that we could use to advance care in epilepsy as well.”
Advertisement
Guidance from the largest cohort of SEEG-confirmed insular epilepsy patients reported to date
Ethical guidance provides guardrails so medical advances benefit patients
OCEANIC-STROKE results represent long-sought advance in secondary stroke prevention
Two studies from Cleveland Clinic may help advance the technology toward broader clinical use
Distinct MRI signature includes lesions beyond the corpus callosum, features predictive of vision and hearing loss
An argument for clarifying the nomenclature
An expert talks through the benefits, limits and unresolved questions of an evolving technology
Recommendations on identifying and managing neurodevelopmental and related challenges